Lack of sleep and migraine are intimately connected. This exploration delves into the complex relationship between insufficient rest and these debilitating headaches. We’ll uncover potential mechanisms, examine various sleep disorders, and explore how sleep deprivation can trigger migraine attacks.
Understanding the symptoms, diagnosis, and risk factors is crucial for effective management. We’ll explore different treatment options, discuss lifestyle adjustments, and investigate how environmental and dietary factors play a role. Finally, we’ll examine the impact on daily life and provide insights into how to cope with this often challenging combination.
Introduction to Sleep Deprivation and Migraines

Sleep deprivation is a significant risk factor for migraine headaches, impacting millions worldwide. The connection between insufficient sleep and migraine attacks is complex, but research has illuminated potential mechanisms and contributing factors. This exploration delves into the intricate relationship between these two prevalent health concerns.Sleep plays a crucial role in regulating various bodily functions, including the nervous system.
Disruptions in sleep patterns can lead to imbalances in the neurochemicals and hormones that influence pain perception and inflammation, potentially triggering migraine episodes. Understanding these mechanisms is essential for developing effective preventative strategies and interventions.
The Relationship Between Sleep and Migraines
Sleep disturbances are frequently associated with migraine development and exacerbation. The disruption of normal sleep patterns can influence the brain’s sensitivity to pain signals, increasing the likelihood of migraine attacks. This is often observed in individuals with chronic sleep disorders.
Ugh, another migraine. Lack of sleep is definitely a major trigger for me, and I’ve been feeling extra tired lately. It’s interesting how some health conditions seem to connect to others in unexpected ways. For example, some research suggests that hormonal changes, like those managed with testosterone blockers for transgender women , can impact sleep patterns.
I’m definitely going to need to prioritize better sleep habits to keep those migraines at bay. Maybe a magnesium supplement will help.
Potential Mechanisms of Sleep-Triggered Migraines
Several theories explain how sleep deprivation might initiate or worsen migraine attacks. One key mechanism involves the imbalance of neurotransmitters, particularly serotonin. Insufficient sleep can lead to a decrease in serotonin levels, a neurotransmitter that plays a crucial role in regulating pain and mood. This imbalance may make the nervous system more susceptible to pain triggers, thus increasing the risk of migraine.
Furthermore, sleep deprivation can lead to increased levels of stress hormones, like cortisol, which can also contribute to migraine attacks.
Types of Sleep Disorders Contributing to Migraine Risk
Various sleep disorders can contribute to an increased risk of migraine. These include:
- Insomnia: Characterized by difficulty falling asleep or staying asleep, insomnia can disrupt the body’s natural sleep-wake cycle. Chronic insomnia often leads to heightened stress and fatigue, both of which can increase migraine susceptibility.
- Sleep Apnea: This disorder involves pauses in breathing during sleep. The repeated interruptions of breathing can lead to oxygen deprivation, which can cause or worsen migraine episodes. Individuals with sleep apnea often experience excessive daytime sleepiness and fatigue, which can further contribute to migraine attacks.
- Shift Work Sleep Disorder: Individuals with irregular sleep schedules due to shift work often experience significant sleep deprivation, impacting the body’s natural circadian rhythm. This disruption can increase the risk of migraines, as the body struggles to adapt to the altered sleep-wake cycle.
- Restless Legs Syndrome: This neurological disorder is characterized by uncomfortable sensations in the legs, which can disrupt sleep. The frequent leg movements and difficulty falling asleep can increase the risk of migraines, especially when these sleep disturbances become chronic.
Prevalence of Migraines in Relation to Sleep Issues
Studies have shown a strong correlation between sleep disorders and migraine prevalence. A significant portion of individuals who experience migraines also report sleep disturbances, suggesting a direct link between the two. For example, a study by the National Institutes of Health found that individuals with chronic sleep disorders had a 25% higher risk of developing migraine headaches compared to those with regular sleep patterns.
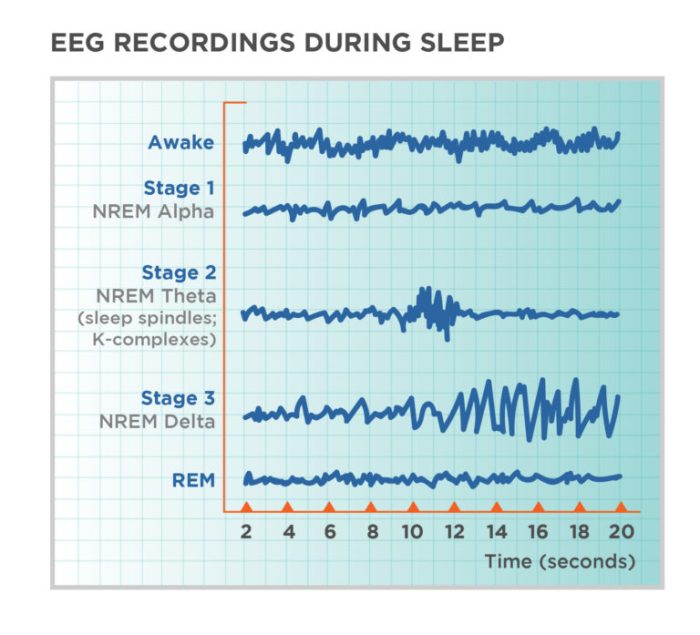
Sleep Stages and Migraine Potential
The following table illustrates the potential connection between sleep stages, duration, and migraine risk.
| Sleep Stage | Duration | Symptoms | Potential Migraine Link |
|---|---|---|---|
| Rapid Eye Movement (REM) | Approximately 20-25% of total sleep time | Dreaming, increased brain activity, rapid eye movements | Disruptions in REM sleep can contribute to migraine attacks, as this stage is crucial for brain restoration and neurotransmitter regulation. |
| Non-REM (Stages 1-4) | Approximately 75-80% of total sleep time | Progressive deepening of sleep; reduced brain activity | Disruptions in any of these stages can result in fragmented sleep and daytime fatigue, which are often associated with migraine attacks. |
| Total Sleep Duration | 7-9 hours per night is ideal | Sufficient rest, mental clarity, and physical well-being | Chronic sleep deprivation can lead to a cascade of negative effects, including increased pain sensitivity, stress, and hormonal imbalances, which can trigger migraines. |
Symptoms and Diagnosis
Understanding the symptoms of sleep deprivation-induced migraines is crucial for accurate diagnosis and effective management. Often, these migraines present with a unique constellation of symptoms that can be subtly different from other types of headaches. Differentiating them requires a keen awareness of the interplay between sleep and pain. A thorough medical history and physical examination are vital steps in the diagnostic process, providing essential context for the individual’s experience.
Common Symptoms of Sleep Deprivation-Induced Migraines
Identifying the specific symptoms associated with sleep deprivation-induced migraines is important for prompt intervention. These symptoms can overlap with other headache types, making accurate diagnosis challenging. Recognizing these nuances is crucial for appropriate treatment.
- Headache intensity and location: Sleep deprivation can exacerbate migraine pain, often manifesting as a throbbing or pulsating sensation, frequently localized to one side of the head.
- Sensitivity to light and sound: These photophobia and phonophobia symptoms are common in migraines, and sleep deprivation can heighten their intensity.
- Nausea and vomiting: Many individuals experience nausea or vomiting alongside the headache pain, which can be severe in cases of sleep deprivation-related migraines.
- Aura: Some individuals may experience an aura, which can include visual disturbances, sensory changes, or other neurological symptoms, before the onset of a migraine. Sleep deprivation can contribute to the development or intensification of this aura.
- Fatigue and mood changes: Sleep deprivation can lead to fatigue, irritability, and difficulty concentrating, which can be significant symptoms in migraine cases. This fatigue can be mistaken for other health issues.
Comparing Sleep Deprivation-Induced Migraines with Other Headache Types
Differentiating sleep deprivation-induced migraines from other headache types is important for effective treatment. Recognizing the specific characteristics of sleep deprivation-related migraines allows for more tailored interventions. Consider the following factors.
- Onset and duration: Sleep deprivation-induced migraines often have a more gradual onset and a longer duration compared to tension headaches. They tend to linger and are often accompanied by a combination of other symptoms.
- Trigger factors: Identifying the triggers is crucial. Sleep deprivation, as opposed to stress or dehydration, can be the key differentiator in some cases.
- Associated symptoms: The presence of fatigue, mood changes, and other neurological symptoms, like an aura, can indicate a potential connection to sleep disturbances.
Diagnostic Process for Migraines Related to Sleep Disturbances
The diagnostic process for migraines linked to sleep disturbances involves a multi-faceted approach, recognizing that sleep deprivation can exacerbate existing migraine patterns. The process emphasizes a careful evaluation.
Ugh, another migraine. Lack of sleep is definitely a culprit, but I’ve been noticing something else lately. Could it be connected to the way my blood sugar fluctuates? Recent research suggests that even in non-diabetics, factors like stress and lack of sleep can trigger a rise in blood sugar levels, potentially contributing to my headaches. Understanding the causes blood sugar rise in non diabetics might be key to managing these pesky migraines.
I’m going to look into this further and see if I can find a pattern. Maybe some lifestyle changes are in order.
A thorough medical history is essential, exploring the patient’s sleep patterns, recent stress levels, and any other potential triggers. A physical examination helps rule out other possible causes of headache. Neurological assessments may be necessary to exclude other neurological conditions.
Importance of Medical History and Physical Examination
A complete medical history and a thorough physical examination are crucial in identifying the underlying cause of migraines, particularly those related to sleep disturbances. These procedures provide essential information.
- Identifying potential triggers: A detailed medical history helps uncover possible triggers for the migraines, including sleep deprivation, stress, diet, and environmental factors.
- Rule out other conditions: A physical examination helps rule out other conditions that may mimic migraine symptoms, ensuring that the diagnosis is accurate and specific.
- Develop a personalized treatment plan: The information gathered from the history and physical examination is essential in developing a personalized treatment plan that addresses both the sleep deprivation and the migraine.
Symptom Table
| Symptom | Severity | Duration | Relation to Sleep |
|---|---|---|---|
| Headache | Moderate to Severe | 4-72 hours | Often exacerbated by sleep deprivation |
| Nausea | Mild to Moderate | Variable | Can be present alongside the headache |
| Photophobia | Moderate to Severe | Variable | Often intensified during sleep deprivation |
| Phonophobia | Moderate to Severe | Variable | Often intensified during sleep deprivation |
Risk Factors and Prevention
Sleep deprivation is a significant risk factor for migraines, creating a vicious cycle where insufficient sleep triggers migraines, and the pain itself can disrupt sleep. Understanding the factors contributing to this connection is crucial for effective prevention strategies. This knowledge empowers individuals to proactively manage their sleep habits and reduce their migraine susceptibility.Migraines are complex and often influenced by a multitude of factors, making prevention multifaceted.
By addressing potential triggers, such as sleep disturbances, individuals can significantly decrease their migraine frequency and intensity.
Sleep Disturbances and Migraine Risk
Sleep disruptions can manifest in various ways, impacting the quality and quantity of sleep. These disturbances often increase the risk of migraine attacks. Interruptions in sleep patterns, such as inconsistent bedtimes and wake-up times, can disrupt the body’s natural circadian rhythm. This rhythm regulates various physiological processes, including hormone production and pain sensitivity. Disruptions can lead to an imbalance, making individuals more vulnerable to migraine attacks.
Strategies for Preventing Sleep Disturbances
Consistent sleep schedules are fundamental to maintaining a healthy circadian rhythm. Aim for a regular bedtime and wake-up time, even on weekends, to establish a predictable sleep-wake cycle. This regularity helps regulate hormones and promotes better sleep quality.
- Maintaining a consistent sleep schedule, even on weekends, promotes a healthy circadian rhythm.
- Creating a relaxing bedtime routine, such as taking a warm bath or reading a book, can signal to the body that it’s time to wind down.
- Creating a sleep-conducive environment, ensuring the bedroom is dark, quiet, and cool, is vital for optimal sleep quality.
Improving Sleep Hygiene
Establishing good sleep hygiene practices is essential for preventing sleep disturbances. These practices focus on creating an environment conducive to sleep and adopting healthy habits that support restful sleep.
- A regular sleep schedule, a relaxing bedtime routine, and a sleep-conducive bedroom environment are crucial for sleep hygiene.
- Avoiding caffeine and alcohol before bed can minimize disruptions to sleep patterns. These substances can interfere with the body’s natural sleep-wake cycle.
- Regular exercise, but not close to bedtime, promotes better sleep. Physical activity can improve sleep quality, but intense workouts before bed can hinder sleep onset.
Stress Management Techniques
Chronic stress is a well-established migraine trigger. Effective stress management techniques can play a vital role in mitigating migraine risk.
- Stress management techniques, such as meditation, yoga, and deep breathing exercises, can help reduce stress levels.
- Mindfulness practices can help individuals become more aware of their thoughts and emotions, allowing them to better manage stress and its impact on their bodies.
- Engaging in relaxing activities, such as spending time in nature or pursuing hobbies, can also help reduce stress and improve sleep quality.
Creating a Sleep Diary
A sleep diary is a valuable tool for tracking sleep patterns and migraine occurrences. By meticulously recording sleep habits and migraine symptoms, individuals can identify potential patterns and triggers.
- A sleep diary can help track sleep patterns, including sleep duration, bedtime, and wake-up time, as well as any sleep disturbances.
- This detailed record can help individuals recognize correlations between sleep patterns and migraine occurrences, enabling proactive management of sleep and migraine risk.
- The diary should also include information about stress levels, dietary intake, and any other relevant factors.
Treatment and Management
Successfully managing migraines exacerbated by sleep deprivation requires a multifaceted approach targeting both the sleep disturbances and the headache pain. This involves a combination of medical interventions, lifestyle adjustments, and potentially, alternative therapies. The key is to identify the underlying causes of both the sleep problems and the migraines, and to develop a personalized treatment plan.Effective treatment often involves a collaborative effort between the patient, their doctor, and potentially other healthcare professionals.
Understanding the interplay between sleep and migraine triggers is crucial for developing a successful management strategy.
Medication Strategies
Medication plays a significant role in managing both the sleep disturbances and the migraine attacks themselves. Over-the-counter pain relievers like ibuprofen or naproxen can help alleviate migraine pain. However, for more severe or frequent migraines, prescription medications, including triptans, may be necessary. These medications work by constricting blood vessels in the brain, reducing inflammation, and easing pain.
Some triptans are available as nasal sprays, making them suitable for quick administration during an attack.Prescription sleep medications can be beneficial in addressing sleep problems contributing to migraine frequency. However, the selection of a sleep medication depends on the underlying cause of the sleep disturbance. A healthcare professional can assess individual needs and prescribe appropriate medication. It’s essential to follow the prescribed dosage and consult a doctor if side effects arise.
Alternative and Complementary Therapies
Alternative and complementary therapies can offer supportive strategies for managing both sleep and migraine symptoms. Relaxation techniques like progressive muscle relaxation or deep breathing exercises can help reduce stress and promote better sleep. Acupuncture and biofeedback therapy are other possibilities, although more research is needed to fully understand their efficacy in managing migraines.These therapies can complement conventional medical approaches and potentially reduce reliance on medication.
It’s vital to discuss any alternative therapy with a healthcare provider before incorporating it into a treatment plan.
Lifestyle Adjustments
Implementing lifestyle adjustments can significantly impact both sleep quality and migraine frequency. Establishing a regular sleep schedule, even on weekends, is crucial for regulating the body’s natural sleep-wake cycle. Creating a relaxing bedtime routine, including avoiding screen time before bed, can also contribute to better sleep.A balanced diet rich in fruits, vegetables, and whole grains, combined with regular exercise, can help improve overall health and reduce migraine triggers.
Managing stress through techniques like yoga or meditation can also be beneficial. Identifying and avoiding known migraine triggers, such as certain foods, environmental factors, or stress-inducing situations, is another essential lifestyle adjustment.
Treatment Comparison Table
| Treatment Type | Mechanism | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Over-the-counter pain relievers (e.g., ibuprofen) | Reduce inflammation and pain | Generally effective for mild to moderate migraines | Stomach upset, allergic reactions (in some cases) |
| Prescription triptans | Constrict blood vessels in the brain, reduce inflammation | Effective for treating acute migraine attacks | Nausea, dizziness, feelings of pressure in the chest |
| Prescription sleep medications | Address sleep disturbances, promote sleep | Variable effectiveness depending on the individual and the underlying sleep problem | Drowsiness, dizziness, dependence |
| Relaxation techniques (e.g., deep breathing) | Reduce stress, promote relaxation | Helpful in managing stress-related migraines and improving sleep quality | Generally low side effects |
Impact on Daily Life
The relentless cycle of sleep-related migraines can severely impact daily life, affecting not just physical well-being but also emotional and mental states. The constant struggle to maintain productivity and engage in social activities can be profoundly challenging. This section will delve into the multifaceted impact of these debilitating conditions, highlighting the strategies individuals employ to cope and navigate their daily routines.The interplay between sleep deprivation and migraine attacks creates a vicious cycle.
Migraines can disrupt sleep, leading to fatigue and further vulnerability to future migraines. This recurring pattern can significantly diminish quality of life, impacting both professional and personal spheres. Understanding these impacts is crucial for developing effective strategies for managing these conditions.
Impact on Daily Activities and Productivity
Sleep-related migraines often lead to reduced concentration, impaired memory, and decreased cognitive function. This can translate to decreased productivity at work or school, as well as difficulty completing daily tasks. Simple activities like reading, focusing on a project, or engaging in conversations can become challenging. For example, an individual experiencing a migraine may struggle to maintain focus during a meeting, leading to missed deadlines or reduced efficiency.
Ugh, another migraine. Lack of sleep is definitely a major trigger. I’ve been trying to incorporate more healthy habits, like taking fish oil supplements, but I’m curious about how long they actually stay in your system. According to this helpful resource, how long does fish oil stay in your system , it seems the duration varies, which is something to keep in mind when you’re trying to make the most of them.
Hopefully, with more consistency and a better sleep schedule, I can avoid these pesky migraines. Wish me luck!
Similarly, students may find it hard to concentrate in class, impacting their academic performance.
Emotional and Psychological Effects
Frequent migraine attacks can have profound emotional and psychological effects. The pain, nausea, and sensitivity to light and sound can lead to feelings of frustration, anxiety, and depression. The unpredictable nature of these attacks can contribute to feelings of helplessness and isolation. For instance, an individual experiencing chronic migraine might avoid social gatherings or activities, fearing a potential attack, impacting their social life.
This isolation can further contribute to negative emotions.
Challenges Faced by Individuals Experiencing Both Sleep Disorders and Migraines
Individuals suffering from both sleep disorders and migraines face a particularly complex set of challenges. The co-occurrence of these conditions often exacerbates symptoms and complicates treatment. The overlapping nature of symptoms can make it difficult to pinpoint the root cause of the problem, delaying effective intervention. For example, insomnia might be misdiagnosed as a migraine symptom, hindering proper treatment for both.
This further emphasizes the importance of a comprehensive diagnosis and tailored management plan.
Strategies for Coping with the Challenges of Migraine-Related Sleep Deprivation
Effective coping strategies for managing migraine-related sleep deprivation involve a multifaceted approach. These include lifestyle adjustments, stress management techniques, and proactive communication with healthcare professionals. Maintaining a consistent sleep schedule, adopting relaxation exercises, and exploring alternative pain relief methods can help break the cycle. Identifying triggers and developing avoidance strategies can also be beneficial. For instance, avoiding caffeine or certain foods known to trigger migraines can minimize the frequency of attacks.
Table: Impact of Sleep-Related Migraines on Daily Activities
| Activity | Difficulty Level | Impact on Sleep | Impact on Migraine Frequency |
|---|---|---|---|
| Work/School | High | Reduced ability to concentrate, increased fatigue | Increased likelihood of attacks, missed deadlines |
| Social Activities | Moderate to High | Avoidance of social gatherings, increased isolation | Potential stress triggers, exacerbation of attacks |
| Household Chores | Moderate | Difficulty maintaining energy levels, fatigue | Increased likelihood of attacks during stressful periods |
| Personal Care | Moderate to High | Disrupted sleep patterns, reduced motivation | Increased sensitivity to triggers, potential for more attacks |
Illustrative Cases
Understanding the link between sleep deprivation and migraines requires looking at real-life examples. These cases highlight the importance of a holistic approach to migraine management, emphasizing the critical role of sleep hygiene in preventing and treating these debilitating headaches. By examining individual experiences, we can better grasp the complex interplay of factors that contribute to migraine episodes.
A Case Study: Sarah’s Struggle
Sarah, a 32-year-old graphic designer, frequently experienced debilitating migraines. Her migraines were often preceded by periods of intense sleep deprivation, typically resulting from late-night work deadlines and social engagements. Her medical history revealed a general tendency toward anxiety and stress, which further complicated her sleep patterns.
Patient Profile
Sarah’s sleep patterns were characterized by inconsistent bedtimes and wake-up times, often staying up late and waking up at different hours each day. She reported difficulty falling asleep and staying asleep, leading to significant daytime fatigue. Migraine triggers for Sarah included caffeine withdrawal, stress, and even bright lights. This combination of factors often resulted in severe migraine episodes.
| Category | Details | Impact | Intervention |
|---|---|---|---|
| Medical History | Anxiety, general stress, occasional insomnia | Increased susceptibility to migraines, difficulty relaxing and falling asleep | Stress management techniques, anxiety medication (with doctor’s approval) |
| Sleep Patterns | Inconsistent sleep schedule, difficulty falling asleep, frequent wake-ups | Significant daytime fatigue, contributing to migraine frequency and severity | Establishing a regular sleep schedule, relaxation exercises before bed, sleep hygiene education |
| Migraine Triggers | Caffeine withdrawal, stress, bright lights, intense work deadlines | Predictable patterns linking triggers to migraine attacks | Avoiding triggers where possible, identifying and managing stress, and practicing mindfulness techniques |
| Dietary Habits | Irregular meals, caffeine intake varies, skipping meals | Contributing to fluctuating energy levels and potential migraine triggers | Regular meal times, balanced diet, managing caffeine intake |
Improving Sleep and Migraine Symptoms
Working with a healthcare professional, Sarah implemented several strategies to improve her sleep and manage her migraines. This included establishing a regular sleep schedule, practicing relaxation techniques like deep breathing and progressive muscle relaxation before bed, and avoiding screen time before sleep. She also learned to manage stress through mindfulness exercises and time management techniques. These strategies, coupled with her doctor’s guidance on migraine prevention medication, significantly reduced the frequency and intensity of her migraine episodes.
“A consistent sleep schedule was the most significant change. It helped regulate my hormones and overall mood, which in turn lessened the migraine triggers.” – Sarah
Holistic Approach
The case of Sarah underscores the importance of a holistic approach to migraine management. It emphasizes that migraines are not isolated events but are often interconnected with other aspects of health, including sleep, stress, and diet. Addressing these interconnected factors is crucial for achieving lasting relief.
Dietary Considerations: Lack Of Sleep And Migraine
Food plays a crucial role in managing both sleep and migraines. What we eat directly impacts our bodies’ ability to regulate hormones, produce energy, and repair tissues, all of which are essential for healthy sleep and a reduction in migraine triggers. Understanding how specific foods affect your sleep patterns and migraine susceptibility can significantly improve your overall well-being.Dietary choices can have a powerful impact on our sleep quality and migraine frequency.
For instance, a diet rich in processed foods and sugary drinks can contribute to disrupted sleep cycles and heightened migraine risk. Conversely, a balanced diet with sufficient nutrients and proper hydration can promote better sleep and reduce the intensity and frequency of migraines.
Influence of Diet on Sleep
A diet rich in complex carbohydrates, lean proteins, and healthy fats can promote better sleep. These nutrients provide sustained energy release, reducing the likelihood of mid-night cravings or energy crashes that disrupt sleep. Foods high in simple sugars, on the other hand, can lead to a spike and subsequent crash in blood sugar, resulting in interrupted sleep. Consuming caffeine and alcohol close to bedtime can also interfere with sleep quality, often leading to a restless night.
Influence of Diet on Migraines
Certain foods and drinks are known migraine triggers. These can include aged cheeses, processed meats, chocolate, caffeine, and alcohol. The individual responses to these triggers vary greatly. Understanding your personal triggers is essential in preventing migraines. Avoiding or minimizing these triggers can significantly reduce the frequency and intensity of migraine attacks.
Food Sensitivities and Sleep-Related Migraines, Lack of sleep and migraine
Food sensitivities, often overlooked, can contribute to both sleep disturbances and migraines. These sensitivities can manifest as digestive issues, fatigue, and mood swings, which can directly affect sleep patterns and increase the likelihood of a migraine attack. Identifying and avoiding these sensitivities is critical for improved sleep and migraine management. A food sensitivity or intolerance can trigger an inflammatory response in the body, contributing to both sleep problems and migraine attacks.
Importance of Hydration
Adequate hydration is crucial for both sleep quality and migraine prevention. Dehydration can lead to headaches and a reduction in blood flow to the brain, which can trigger or worsen migraines. Staying well-hydrated throughout the day, especially during sleep, is vital for maintaining optimal body function. It is essential to drink plenty of water throughout the day to ensure adequate hydration and maintain overall health.
Dietary Recommendations
A balanced diet rich in fruits, vegetables, whole grains, and lean proteins is generally recommended for better sleep and migraine management. This approach provides the necessary nutrients to support healthy bodily functions, including proper brain and nervous system function.
Relationship between Food Sensitivities and Sleep-Related Migraines
Individuals with food sensitivities may experience migraine attacks related to sleep deprivation. For instance, a food intolerance may cause digestive discomfort, which can disrupt sleep and increase the risk of a migraine attack. This relationship is complex, highlighting the interplay between diet, sleep, and migraines.
Importance of Hydration
Adequate hydration is essential for maintaining proper bodily functions and reducing the likelihood of migraines. Drinking enough water can help regulate blood flow to the brain, preventing dehydration-related headaches. Staying well-hydrated is critical for sleep quality, as dehydration can lead to discomfort and restlessness, interfering with sleep cycles.
Dietary Considerations Table
| Food | Effect on Sleep | Effect on Migraines | Potential Interactions |
|---|---|---|---|
| Processed Foods | Can disrupt sleep cycles due to high sugar content and poor nutrient composition. | Often a trigger for migraines due to inflammatory compounds and additives. | Increased risk of sleep disturbances and migraines, especially when consumed in large quantities. |
| Caffeine | Can cause insomnia and restless sleep if consumed close to bedtime. | Known migraine trigger, exacerbating existing symptoms in susceptible individuals. | Caffeine withdrawal can lead to headaches, making it crucial to consume it in moderation. |
| Alcohol | Disrupts sleep cycles, leading to fragmented and less restorative sleep. | Can trigger or worsen migraines in some individuals. | Combination of alcohol and caffeine consumption can intensify negative effects on sleep and migraines. |
| Fruits and Vegetables | Provide essential vitamins and minerals for better sleep regulation. | Generally considered safe and can contribute to overall health, potentially reducing migraine risk. | No significant negative interactions, but consider individual sensitivities. |
Environmental Factors
Our environment plays a significant role in both sleep quality and migraine triggers. From the comforting quiet of a dark room to the disruptive chaos of a noisy city, external factors can dramatically influence our bodies’ ability to rest and recover. Understanding these influences is key to managing both sleep deprivation and migraine headaches effectively.
Impact of Environmental Noise
Noise pollution, a common feature of modern life, can significantly disrupt sleep patterns. Constant background noise, whether from traffic, construction, or even household appliances, can make it difficult to fall asleep and stay asleep. This constant stimulation interferes with the natural sleep cycles, leading to fragmented sleep and reduced sleep quality. The resulting sleep deprivation can exacerbate migraine symptoms.
Studies have shown a correlation between noise levels and migraine frequency, with higher noise levels often linked to more frequent attacks. A quiet environment is crucial for restful sleep, allowing the body to repair and rejuvenate. The absence of distracting noises creates a conducive atmosphere for better sleep and reduced migraine episodes.
Importance of Darkness and Light Exposure
Melatonin, a hormone crucial for regulating sleep-wake cycles, is significantly affected by light exposure. Exposure to bright light, especially in the evening, can suppress melatonin production, making it harder to fall asleep. Conversely, a dark environment promotes melatonin production, facilitating a smoother transition into sleep. Consistent light exposure, including exposure to artificial light sources at night, can disrupt the natural circadian rhythm and increase the likelihood of migraine attacks.
This disruption of the body’s internal clock can manifest as a significant contributor to the onset of migraines.
Impact of Temperature and Humidity
Temperature and humidity levels in the sleep environment can significantly impact sleep quality. A consistently cool room temperature is often preferred for optimal sleep. Extreme temperatures, whether too hot or too cold, can disrupt sleep, leading to restlessness and discomfort. Similarly, high humidity can make the environment feel stuffy and uncomfortable, affecting sleep quality and potentially triggering migraines.
Conversely, extremely low humidity can cause dryness, potentially contributing to headaches and migraines. The ideal temperature range for sleep varies from person to person, but generally, a cool and dry environment is most conducive to restful sleep and reduced migraine risk.
Environmental Factors Affecting Sleep and Migraines
| Environmental Factor | Impact on Sleep | Impact on Migraines | Mitigation Strategies |
|---|---|---|---|
| Noise Pollution | Disrupted sleep cycles, fragmented sleep, reduced sleep quality | Increased migraine frequency and severity | Use earplugs, white noise machines, soundproof curtains, relocate to a quieter area, or request noise reduction in the environment. |
| Light Exposure | Suppressed melatonin production, difficulty falling asleep, poor sleep quality | Increased migraine frequency and severity, particularly with inconsistent light exposure | Use blackout curtains, eye masks, or sleep shades. Establish a consistent sleep schedule, including consistent sleep and wake times, and limit screen time before bed. |
| Temperature | Discomfort, restlessness, difficulty falling asleep, poor sleep quality | Possible triggers or exacerbations, depending on individual sensitivity | Maintain a cool room temperature. Use fans or air conditioning to regulate the temperature. |
| Humidity | Stuffy environment, discomfort, difficulty breathing | Possible triggers or exacerbations, depending on individual sensitivity | Use a dehumidifier to maintain a comfortable level of humidity, especially during periods of high humidity. Ensure proper ventilation in the sleeping area. |
Concluding Remarks
In conclusion, the link between lack of sleep and migraine is undeniable. By understanding the mechanisms, recognizing symptoms, and implementing preventative strategies, individuals can take proactive steps towards better sleep hygiene and reduced migraine frequency. A holistic approach, encompassing lifestyle adjustments, dietary considerations, and environmental modifications, can significantly improve overall well-being and quality of life.









