Living with a pacemaker is a significant life change, but it doesn’t have to be daunting. This guide delves into the practical and emotional aspects of navigating daily life with a pacemaker, from understanding its function to managing potential complications. We’ll cover everything from the basics of pacemaker technology to the importance of routine medical check-ups and emotional well-being.
From the intricate workings of the device itself to the adjustments required in daily life, we’ll provide a thorough overview. We’ll also explore the emotional and social impacts of living with a pacemaker, highlighting the importance of support networks and practical strategies.
Understanding Pacemaker Function
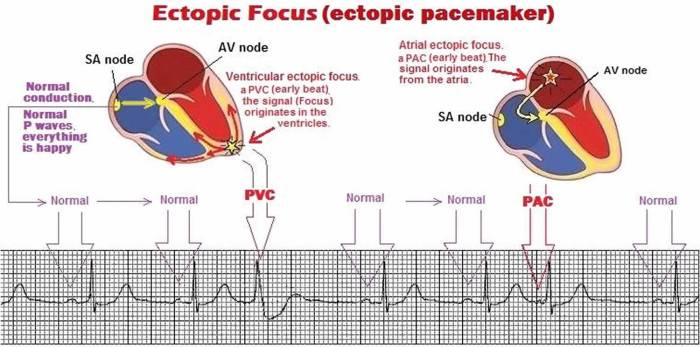
A pacemaker is a small device that helps regulate the heartbeat. It’s a critical component for individuals with heart conditions that cause abnormal heart rhythms. Understanding its function, components, and types is essential for anyone living with a pacemaker or considering this option.The basic mechanism of a pacemaker involves detecting and responding to electrical signals from the heart.
When the heart’s natural electrical system malfunctions, the pacemaker steps in to maintain a consistent and healthy heart rate.
Pacemaker Components
Pacemakers are sophisticated medical devices. They consist of a pulse generator and one or more pacing leads. The pulse generator is the “brain” of the device, housing the battery, circuitry, and the microprocessor that controls the timing and strength of the electrical impulses. The pacing leads are thin wires that are threaded into the heart chambers, delivering the electrical impulses to the heart muscle to stimulate a beat.
The leads are insulated and coated to prevent the body from rejecting them.
Pacemaker Types
Different types of pacemakers cater to various heart conditions and individual needs. These devices vary in their capabilities and programming.
- Single-chamber pacemakers: These pacemakers stimulate a single chamber of the heart (typically the lower chamber, the ventricle). They are often used for simple rhythm disturbances.
- Dual-chamber pacemakers: These pacemakers stimulate both the atria and the ventricles of the heart. They are more complex, coordinating both the upper and lower chambers for a more natural heartbeat.
- Triple-chamber pacemakers: These are less common and are used for complex heart conditions requiring stimulation of the right atrium, the left atrium, and the ventricle. This type of pacemaker is designed to help synchronize the activity of different parts of the heart more precisely.
- Biventricular pacemakers: These devices are a type of dual-chamber pacemaker that specifically stimulate both ventricles. This can improve heart function in patients with heart failure.
Temporary vs. Permanent Pacemakers
The choice between a temporary and permanent pacemaker depends on the patient’s condition and the expected duration of treatment.
- Temporary pacemakers: These pacemakers are used for short-term support, often during a hospital stay. They are often connected via wires to an external power source. Temporary pacemakers are frequently employed during procedures or when a patient’s heart rhythm is unstable and requires immediate intervention.
- Permanent pacemakers: These pacemakers are implanted under the skin, typically under the collarbone, and are designed for long-term use. They have a battery that powers the device, which will last for several years.
Pacemaker Placement
 (Diagram placeholder. A permanent pacemaker is typically implanted under the skin near the collarbone, with thin wires (leads) extending to the heart chambers. The pulse generator is housed within the implanted casing.)
(Diagram placeholder. A permanent pacemaker is typically implanted under the skin near the collarbone, with thin wires (leads) extending to the heart chambers. The pulse generator is housed within the implanted casing.)
Electrical Signals in Pacemaker Operation
The pacemaker’s operation relies on precise timing of electrical signals. The device monitors the heart’s electrical activity. When the heart’s natural rhythm is too slow or irregular, the pacemaker sends an electrical impulse to stimulate the heart muscle to contract, thus regulating the heart rate. This ensures the heart beats at a stable and healthy pace.
The electrical signals from the pacemaker are carefully programmed to deliver precise impulses at specific intervals, optimizing the heart’s rhythm.
Daily Life with a Pacemaker
Adjusting to life with a pacemaker involves more than just getting used to the device. It’s about understanding how it affects daily activities, lifestyle choices, and overall well-being. This transition period requires careful consideration of potential limitations and the importance of ongoing medical care.Living with a pacemaker requires some adjustments to daily routines and activities, but it doesn’t necessarily mean a complete lifestyle overhaul.
Many people with pacemakers lead fulfilling lives, engaging in a wide range of activities. The key is understanding the device’s impact and making informed decisions.
Impact on Daily Activities
Understanding how a pacemaker influences daily routines is crucial. Certain activities may require modification or consideration. Heavy lifting, vigorous exercise, and prolonged periods of strenuous activity may need adjustments. However, most people with pacemakers can maintain a largely normal activity level. Light to moderate exercise is usually encouraged, and individual needs should be discussed with the healthcare provider.
Lifestyle Choices and Considerations
Certain lifestyle choices may need slight modifications. For example, activities involving significant electromagnetic fields, like close proximity to large electrical equipment or high-frequency devices, should be discussed with a healthcare provider. The impact on certain activities, like driving, should be evaluated by the physician and state-specific regulations should be followed. This will ensure safety and compliance.
Potential Limitations and Restrictions
While pacemakers significantly improve quality of life, they do impose some limitations. These restrictions are usually specific to the individual and depend on the type of pacemaker and the patient’s overall health. Some individuals may experience a slightly decreased tolerance to extreme temperatures, and some may have restrictions on specific types of work, which is typically assessed on a case-by-case basis.
Living with a pacemaker is a significant adjustment, but navigating the challenges is definitely manageable. Weighing the pros and cons of medical procedures like a tonsillectomy can be tricky, especially when considering the potential risks and benefits. For example, exploring the decision-making process surrounding a tonsillectomy, and whether it’s the right choice, is crucial, as detailed in this informative article on tonsillectomy risks versus benefits is it worth it.
Ultimately, making informed decisions about your health, whether it’s managing a pacemaker or facing other medical choices, is key to living a fulfilling life.
Comparison to Life Without a Pacemaker
The experience of living with a pacemaker is distinct from life without one. It’s crucial to understand that while some adjustments are necessary, many people with pacemakers can lead active, fulfilling lives. The pacemaker helps maintain a normal heart rhythm, improving quality of life, and allowing for activities previously hindered by heart conditions. The focus should be on living a healthy life while understanding the unique needs of the device.
Importance of Routine Medical Check-ups
Regular medical check-ups are paramount for pacemaker patients. These check-ups allow for monitoring of pacemaker function, detection of any potential complications, and adjustments to programming as needed. Regular follow-ups are essential for ensuring the pacemaker continues to operate optimally and that any issues are identified and addressed promptly. These visits also offer a chance to discuss any concerns or questions related to daily living and the pacemaker’s impact.
Medical Procedures and Care: Living With A Pacemaker
Living with a pacemaker requires understanding the procedures involved in implantation, follow-up care, and potential complications. This knowledge empowers individuals to actively participate in their health management and ensures they receive the best possible care. A proactive approach to pacemaker management minimizes risks and maximizes the device’s effectiveness.The pacemaker implantation procedure is a carefully orchestrated process involving several stages.
Prior to the procedure, thorough medical evaluations are conducted to assess patient health, identify any potential risks, and ensure the pacemaker is the most appropriate solution.
Pacemaker Implantation Procedure
The procedure itself typically involves a small incision, often in the chest, to access the heart. Under sterile conditions and using precise surgical techniques, the pacemaker is implanted beneath the skin, connected to the heart’s electrical system. This connection is crucial for the pacemaker to effectively regulate the heart’s rhythm. Anesthesia is administered to ensure patient comfort throughout the procedure.
Pre-Operative Care
Before the implantation, patients are advised to follow a specific pre-operative care regimen. This includes fasting for a certain period before the procedure and abstaining from certain medications. Strict adherence to these instructions is essential to minimize potential complications.
Post-Operative Care
Following the implantation, patients are closely monitored for any signs of complications. Rest is crucial in the initial recovery period. Patients are typically instructed on how to care for the incision site and manage any discomfort. Pain medication is often prescribed to alleviate post-operative pain.
Follow-up Appointments and Monitoring
Regular follow-up appointments are essential for monitoring the pacemaker’s function and ensuring proper device performance. These appointments allow healthcare professionals to assess the pacemaker’s settings, evaluate the patient’s overall health, and detect any potential issues early.
Common Complications
- Infection at the incision site: Prompt medical attention is critical to address any signs of infection, such as redness, swelling, or discharge. Antibiotics are usually prescribed to manage the infection effectively.
- Blood clots: The risk of blood clots forming in the legs or lungs is a concern after any surgical procedure. Medication and movement exercises are often recommended to mitigate this risk.
- Pacemaker malfunction: The pacemaker may malfunction due to various reasons. Regular checkups and monitoring are crucial to detect and address these issues quickly.
- Electrode dislodgement: This can lead to irregular heart rhythms. Regular monitoring and appropriate adjustments to the pacemaker’s settings are crucial.
Managing Potential Side Effects or Complications
Open communication with the healthcare team is vital for promptly addressing any concerns. Patients should report any unusual symptoms, such as chest pain, dizziness, or shortness of breath. These symptoms might indicate a problem that requires immediate medical attention.
Adherence to Prescribed Medication Regimens
Adherence to the prescribed medication regimen is critical for optimal pacemaker function and overall health. This includes taking medication as directed, understanding the purpose of each medication, and reporting any side effects to the healthcare team.
Medication regimens should be meticulously followed to ensure the pacemaker operates correctly and to manage any potential health issues.
Emotional and Psychological Impact
Living with a pacemaker is a significant life change, impacting not only physical health but also emotional well-being. Patients may experience a range of feelings, from initial anxiety and fear to adjustments and acceptance. Understanding these emotional responses is crucial for providing comprehensive care and support.Adjusting to a pacemaker requires acknowledging the physical and emotional changes it brings.
Patients may feel a sense of vulnerability or dependence on the device, which can be a source of anxiety. The need for regular check-ups and potential complications further contributes to this emotional landscape.
Emotional Challenges Associated with Pacemaker Implantation
The emotional journey often starts with anxiety about the procedure itself. Patients may worry about pain, discomfort, or the unknown. This anxiety can extend to the long-term implications of living with a pacemaker, including potential limitations or changes in lifestyle. These feelings are completely normal and understandable. Patients might also experience fear of complications, like device malfunction or infection.
Importance of Support Networks
Strong support networks are vital for managing the emotional challenges. Family, friends, and support groups provide a sense of belonging and understanding. Sharing experiences and coping strategies with others facing similar situations can be extremely beneficial. The encouragement and reassurance from a supportive network can significantly impact a patient’s emotional well-being.
Coping Mechanisms for Managing Stress and Anxiety
Several coping mechanisms can help patients navigate the emotional landscape. These include mindfulness practices, such as meditation or deep breathing exercises, to manage stress and anxiety. Engaging in hobbies and activities that bring joy and relaxation can also help maintain emotional equilibrium. Seeking professional help from a therapist or counselor is another crucial option, particularly for more intense or persistent feelings of anxiety or depression.
Journaling can be a helpful tool for processing emotions and reflecting on adjustments.
Resources for Emotional Support
Numerous resources are available to support pacemaker patients. These include support groups offered by medical centers or community organizations. Online forums dedicated to patients with pacemakers can provide a sense of community and allow for peer-to-peer support. Mental health professionals can offer guidance and therapy to help patients cope with anxiety and depression. Hospitals and clinics often have dedicated social workers or counselors who can connect patients with appropriate resources.
Comparison of Emotional Responses Across Age Groups
| Age Group | Common Emotions | Coping Strategies | Support Resources |
|---|---|---|---|
| Children/Adolescents | Fear of the unknown, anxiety about the device’s appearance, social concerns about peers’ reactions, difficulty adjusting to activity limitations | Positive reinforcement from caregivers, engaging in age-appropriate activities, providing clear and age-appropriate explanations, creating a supportive and understanding environment, participation in support groups for adolescents with medical devices. | Support groups for pediatric cardiac patients, counselors specializing in adolescent mental health, family therapists, social workers. |
| Young Adults | Uncertainty about future plans, anxiety about career prospects, fear of social stigma, adjusting to lifestyle changes, body image concerns. | Seeking information about the pacemaker and its implications, setting realistic goals, engaging in activities that provide emotional support, connecting with peers facing similar challenges, exploring career options that align with the pacemaker. | Support groups for young adults with medical devices, career counseling services, mental health professionals specializing in young adult issues, patient advocacy groups. |
| Middle-aged Adults | Fear of the impact on family responsibilities, concern about maintaining work/life balance, anxiety about potential future limitations, financial anxieties | Open communication with family members, prioritizing self-care, exploring support groups, seeking professional guidance, managing expectations and setting realistic goals. | Support groups for middle-aged adults with medical conditions, financial advisors, family therapists, support groups specifically tailored for cardiac patients. |
| Seniors | Fear of losing independence, concern about the device’s maintenance, anxiety about the potential for complications, adjustment to changes in mobility | Focusing on strengths and abilities, maintaining social connections, seeking assistance from family and friends, prioritizing physical activity within limitations, participating in community activities. | Senior centers offering support groups, geriatric care facilities with social workers, home health aides, support groups for older adults with medical devices. |
Social and Practical Considerations
Living with a pacemaker can impact various aspects of daily life, from social interactions to practical tasks. Understanding these considerations empowers individuals to navigate these changes effectively and maintain a fulfilling life. This section explores the nuances of social situations, practical strategies, and the importance of educating others about pacemakers.
Social Situations and Interactions
Social situations can sometimes present challenges when living with a pacemaker. For example, individuals might experience concerns about potential misunderstandings or judgments from others regarding their medical device. These concerns can stem from a lack of awareness or knowledge about pacemakers. It is crucial to approach social interactions with confidence and proactively address any questions or concerns others may have.
Strategies for Managing Social Interactions
Effective communication and preparation are key to managing social interactions. Openly discussing the pacemaker with friends, family, and colleagues can alleviate anxieties and promote understanding. Providing simple explanations, such as “I have a pacemaker for [reason],” can foster a more comfortable environment for conversations.
Educating Others about Pacemakers
Educating others about pacemakers is crucial for fostering understanding and reducing misconceptions. Sharing information about the device’s function, its impact on daily life, and common concerns can help others appreciate the situation and offer support. A well-prepared explanation can alleviate potential anxieties and ensure smoother social interactions.
Practical Tips for Managing Daily Tasks and Activities
Managing daily tasks and activities with a pacemaker requires thoughtful planning and adaptation. Understanding the limitations of the device, such as the need to avoid certain types of activities, is essential. Individuals can use a calendar to schedule appointments and tasks, which can help maintain a structured daily routine. Regular exercise and a healthy lifestyle are important for overall well-being and can help manage the impact of the pacemaker on daily life.
Impact of a Pacemaker on Different Aspects of Life
| Aspect of Life | Impact | Strategies | Resources |
|---|---|---|---|
| Social Interactions | Potential for misunderstandings, concerns from others. | Open communication, providing clear explanations, seeking support from others. | Support groups, online forums. |
| Employment | Potential for workplace accommodations, need for disclosure. | Communicating with employer, obtaining necessary accommodations. | Employee Assistance Programs (EAPs). |
| Travel | Potential need for medical documentation, information about pacemaker. | Packing necessary medical documentation, informing travel companions. | Travel medicine clinics, airline personnel. |
| Physical Activities | Potential limitations, need for adjustments to routine. | Consult with healthcare professional, gradual introduction to activities. | Physical therapists, fitness instructors. |
| Healthcare | Regular checkups, follow-up appointments. | Scheduling appointments, adherence to medical recommendations. | Healthcare providers, insurance companies. |
Diet and Exercise
Living with a pacemaker doesn’t mean a complete overhaul of your lifestyle. A balanced approach to diet and exercise can significantly improve your overall well-being and ensure your pacemaker functions optimally. It’s important to remember that specific recommendations may vary based on individual circumstances, so it’s crucial to discuss these with your doctor.Maintaining a healthy weight and lifestyle is vital for overall health, regardless of having a pacemaker.
This includes a balanced diet and regular exercise. These choices support a stronger immune system, potentially reduce the risk of complications, and improve energy levels. The combination of both diet and exercise significantly impacts the effectiveness and longevity of the pacemaker’s function.
Living with a pacemaker can be a bit of a lifestyle adjustment, but I’ve found some surprising ways to maintain good health. For example, taking care of my skin has become extra important, and I’ve been really enjoying using salt water for the face salt water for the face as a gentle cleanser. It’s a simple, natural way to keep my skin feeling refreshed, which helps me feel better overall, especially when I’m adjusting to having a pacemaker.
Dietary Recommendations
A healthy diet plays a crucial role in managing overall health and supporting the pacemaker. It’s recommended to focus on a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. Limit processed foods, sugary drinks, and excessive saturated and unhealthy fats. A balanced approach provides essential nutrients without putting unnecessary stress on the body.
- Focus on nutrient-dense foods: Fruits, vegetables, lean proteins, and whole grains are excellent choices. They provide essential vitamins, minerals, and fiber, supporting overall health and potentially reducing the risk of complications.
- Limit processed foods: These often contain high levels of sodium, unhealthy fats, and added sugars. These can contribute to weight gain and potential health issues, which can, in turn, affect pacemaker function indirectly.
- Hydration is key: Adequate water intake is essential for overall health. This includes water, unsweetened beverages, and other suitable liquids.
- Consult with a registered dietitian: A registered dietitian can provide personalized dietary recommendations based on your specific needs and medical conditions. This personalized approach is important to consider.
Exercise Guidelines
Regular exercise is crucial for maintaining physical health and well-being. A pacemaker doesn’t prohibit exercise; it simply requires careful consideration of the type and intensity of activity. It’s essential to consult your doctor before starting or modifying any exercise routine.
- Start slowly and gradually increase intensity: Begin with low-impact activities and gradually increase the duration and intensity of exercise as your fitness improves. This gradual approach helps prevent undue stress on the body.
- Avoid high-impact activities: Activities that involve sudden changes in direction or high-impact movements can potentially disrupt the pacemaker’s function. Consider low-impact alternatives like swimming, walking, or cycling.
- Listen to your body: If you experience any unusual symptoms, such as dizziness, lightheadedness, or chest pain, stop exercising immediately and contact your doctor.
- Exercise with caution in extreme temperatures: Extreme heat or cold can affect blood circulation and potentially impact the pacemaker’s performance. Take necessary precautions, such as staying hydrated and exercising indoors during extreme weather.
Potential Medication and Dietary Interactions
Certain medications and dietary choices may interact with each other, affecting their effectiveness. Consult with your doctor about potential interactions.
- Medications can affect nutrient absorption: Some medications can interfere with the absorption of certain nutrients. A doctor can recommend adjustments to ensure proper nutrition.
- Dietary choices can affect medication efficacy: The timing and type of food can impact how effectively certain medications work. Your doctor can advise on optimal intake times.
Adjusting Exercise Routines
Adjusting exercise routines is crucial to ensure safety and optimal pacemaker function.
- Modifying exercise intensity: It’s important to monitor the intensity of your workout to prevent potential stress on the pacemaker. Start slowly and progressively increase intensity to avoid straining your body.
- Consider the environment: Exercise in a controlled environment can prevent unforeseen challenges, such as extreme weather conditions.
Examples of Healthy and Safe Exercises
Examples of safe exercises for pacemaker patients include walking, swimming, cycling, and light weight training. Remember to consult your doctor before starting any new exercise program.
- Walking: A simple and effective way to increase cardiovascular health. Walking at a moderate pace for 30 minutes most days of the week is beneficial.
- Swimming: A low-impact exercise that works many muscle groups. Swimming is a great option for people with pacemakers.
- Cycling: A low-impact cardio exercise that can be performed indoors or outdoors. Cycling is a great choice for maintaining fitness.
- Light weight training: Strength training with light weights can help build muscle and improve overall fitness. Consult your doctor about appropriate weight and resistance levels.
Technological Advancements
Pacemakers have undergone remarkable evolution since their inception, becoming increasingly sophisticated and reliable tools for managing cardiac conditions. This progression has significantly improved the quality of life for millions worldwide, offering hope and effective treatment options for those with compromised heart rhythms.Modern pacemakers are not just simple electrical impulses; they are complex devices capable of adapting to individual patient needs.
The advancements in technology have expanded the capabilities of these devices, leading to better outcomes and enhanced patient comfort. This evolution is a testament to ongoing research and development in the field of cardiology.
Evolution of Pacemaker Technology
Early pacemakers were bulky and required frequent adjustments. Over time, miniaturization and improvements in battery technology allowed for smaller, more discreet devices. The development of implantable pulse generators and sophisticated algorithms for adjusting pacing rates revolutionized the field. Early models were primarily fixed-rate devices, but newer generations are programmed to respond dynamically to the patient’s heart rate and activity levels.
Living with a pacemaker can be a bit of a rollercoaster, honestly. Managing the daily adjustments and routines is key, and finding ways to stay proactive about your health is crucial. This often includes exploring options like a type 2 diabetes cure if it’s something you’re facing, and making sure you’re getting the right support. Ultimately, staying positive and focusing on healthy habits are essential for living your best life with a pacemaker.
Recent Advancements in Pacemaker Design and Functionality
Recent advancements include the integration of more sophisticated sensors that monitor the heart’s electrical activity with greater precision. This leads to more tailored pacing strategies and minimizes unnecessary stimulation. These advancements also improve the accuracy of detecting and responding to arrhythmias. Furthermore, the development of more efficient and longer-lasting battery technologies has extended the intervals between pacemaker replacements, reducing the frequency of invasive procedures.
Different Types of Modern Pacemakers
Modern pacemakers are categorized based on their function and complexity. Single-chamber pacemakers stimulate a single chamber of the heart, while dual-chamber pacemakers coordinate the activity of both the atria and ventricles. Cardiac resynchronization therapy pacemakers (CRT-P) are a specialized type that helps resynchronize the heart’s pumping action, particularly beneficial for patients with heart failure.
Emerging Trends and Future Prospects
Future pacemaker technology is expected to focus on more sophisticated algorithms for adapting to various physiological conditions. Wireless communication and remote monitoring capabilities are being explored to facilitate continuous patient assessment and prompt intervention when necessary. The integration of artificial intelligence (AI) into pacemaker programming is also a promising trend, potentially enabling the devices to predict and prevent future arrhythmias.
Comparison of Pacemaker Technologies
| Technology Type | Benefits | Limitations | Applications |
|---|---|---|---|
| Single-Chamber Pacemaker | Simpler design, lower cost. | May not address complex arrhythmias. | Patients with sinus node dysfunction or simple atrial fibrillation. |
| Dual-Chamber Pacemaker | More comprehensive control of heart rhythm. | Slightly higher risk of complications. | Patients with more complex heart conditions, including AV block. |
| Cardiac Resynchronization Therapy Pacemaker (CRT-P) | Improves heart pumping efficiency, reducing symptoms of heart failure. | More complex implantation, potential for higher device-related complications. | Patients with heart failure and specific electrical conduction abnormalities. |
| Pacemakers with Advanced Algorithms | Tailored pacing strategies, optimized for individual needs. | Requires sophisticated programming and potentially more extensive follow-up. | Patients with a wide range of heart conditions needing individualized pacing solutions. |
Troubleshooting and Emergencies
Living with a pacemaker requires understanding potential issues and knowing how to react in emergencies. This section provides crucial information on recognizing pacemaker malfunction, taking appropriate steps, and accessing emergency resources. Knowing these procedures can significantly impact your well-being and safety.
Recognizing Signs of Pacemaker Malfunction
Pacemaker malfunctions can manifest in various ways. It’s essential to be aware of these signs so you can seek immediate medical attention. Common symptoms include a noticeable change in heart rate, such as a significantly faster or slower pulse than usual. You might experience dizziness, lightheadedness, or fainting spells. Unusual sensations, like palpitations or a fluttering in your chest, are also important to note.
Changes in the pacing rhythm, such as skipping beats or a feeling of a “missed” beat, should also be reported.
Steps to Take in Case of a Suspected Pacemaker Problem, Living with a pacemaker
If you suspect a pacemaker issue, immediate action is crucial. First, remain calm and assess the situation. Note the symptoms, including the time they started and their severity. If possible, document the exact symptoms and the time they started. If you have a medical alert device or a card with your pacemaker information, ensure it’s readily accessible.
Immediately contact your primary care physician or the pacemaker implanting facility. If symptoms are severe, or if you experience chest pain, shortness of breath, or loss of consciousness, call emergency services (e.g., 911 or your local emergency number).
Emergency Contacts and Procedures
Maintaining a list of emergency contacts is vital. This list should include your primary care physician, the pacemaker implanting facility, and family members or friends who can assist. Keep this list readily available and ensure emergency contacts have your pacemaker information. Having your pacemaker’s model number, implant date, and any other relevant details handy will help medical professionals quickly diagnose the issue.
Make sure you have a method to quickly notify your contacts if you are unable to do so yourself.
Common Pacemaker Issues and Their Solutions
Pacemaker malfunctions can arise from various reasons. One common issue is a temporary intermittent malfunction. These often resolve themselves, but immediate medical attention is still recommended. Sometimes, the battery may need replacing. This is a routine procedure, but it is crucial to schedule the replacement with your doctor to prevent complications.
A more serious issue could be a lead dislodgement. This requires immediate medical intervention.
Flowchart of Pacemaker Emergency Procedures
(Note: This is a sample flowchart and cannot be generated without an image or specific formatting requirements. Please replace this with a proper flowchart image or text description outlining the steps in a pacemaker emergency situation.)
The flowchart would visually guide through the steps from recognizing symptoms to contacting emergency services.
Epilogue
Living with a pacemaker is a journey of adaptation and understanding. By exploring the technological advancements, practical considerations, and emotional challenges, this comprehensive guide aims to empower pacemaker recipients and their loved ones. Remember, you’re not alone in this journey, and with the right information and support, you can lead a fulfilling life while managing this important medical device.










