Mean corpuscular hemoglobin concentration (MCHC) paints a crucial picture of red blood cell health. It reveals the average amount of hemoglobin packed within each red blood cell, a vital metric for diagnosing and understanding various hematological conditions. This in-depth exploration will delve into the definition, measurement, interpretation, and clinical applications of MCHC, highlighting its significance in assessing overall blood health.
Understanding MCHC involves looking at how it relates to other blood indices like MCV and MCH. We’ll explore the methodologies used to measure it in a lab setting, discussing the normal ranges, potential abnormalities, and the resulting diagnoses. The information presented here will allow readers to gain a comprehensive understanding of MCHC’s role in the intricate world of hematology.
Mean Corpuscular Hemoglobin Concentration (MCHC)
Mean Corpuscular Hemoglobin Concentration (MCHC) is a crucial blood test parameter that provides insights into the red blood cell’s ability to carry oxygen. It reflects the average concentration of hemoglobin within a single red blood cell. Understanding MCHC values is essential for diagnosing and managing various hematological conditions, helping clinicians assess the overall health of red blood cells.MCHC provides valuable information about the hemoglobin content packed within a given volume of red blood cells.
This parameter is calculated by dividing the total amount of hemoglobin by the total volume of red blood cells. Clinically, MCHC helps evaluate the efficiency of oxygen transport and identify potential abnormalities in red blood cell function.
Definition of MCHC
MCHC, or mean corpuscular hemoglobin concentration, is the average concentration of hemoglobin within a single red blood cell. It’s a critical measure in evaluating red blood cell health. The concentration is expressed in grams per deciliter (g/dL).
Clinical Significance of MCHC
MCHC plays a vital role in assessing red blood cell health and diagnosing various hematological conditions. Anomalies in MCHC often correlate with issues in hemoglobin production, red blood cell production, or red blood cell destruction. For instance, high MCHC suggests an increased hemoglobin concentration within the red blood cells, while low MCHC often indicates a reduced hemoglobin concentration.
Role of MCHC in Diagnosing Hematological Conditions
MCHC abnormalities can point to several hematological conditions. A high MCHC might suggest spherocytosis, a condition where red blood cells are spherical instead of biconcave, leading to increased hemoglobin concentration. Conversely, a low MCHC is frequently observed in conditions like iron deficiency anemia, where inadequate iron impairs hemoglobin production, resulting in lower hemoglobin concentration in the red blood cells.
Mean corpuscular hemoglobin concentration (MCHC) is all about the concentration of hemoglobin within red blood cells. While fascinating, it’s a bit different than what happens if you swallow gum, which, according to this resource ( what happens if you swallow gum ), isn’t usually a major health concern. Ultimately, understanding MCHC helps us understand red blood cell health and function.
Other conditions like thalassemia and sickle cell disease can also affect MCHC levels.
Relationship between MCHC and Other Red Blood Cell Indices
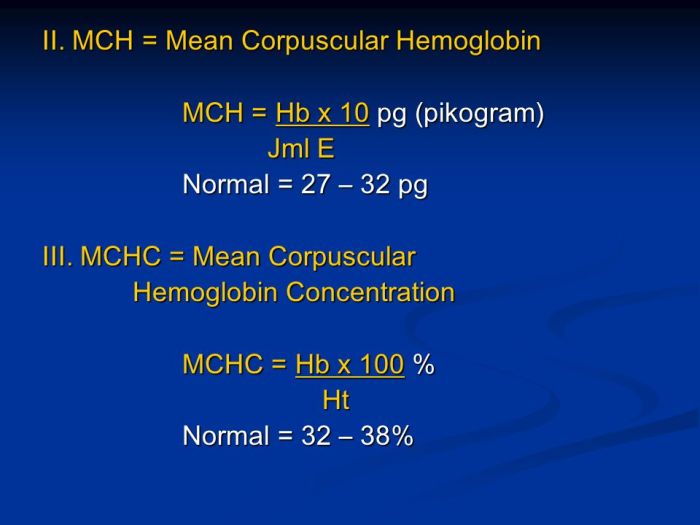
MCHC is closely linked to other red blood cell indices, including Mean Corpuscular Volume (MCV) and Mean Corpuscular Hemoglobin (MCH). These parameters provide a comprehensive picture of red blood cell characteristics. For example, a low MCHC often accompanies low MCH, indicating decreased hemoglobin content per red blood cell. Similarly, the relationship between MCHC and MCV can offer further insights into the underlying causes of hematological disorders.
Mean corpuscular hemoglobin concentration (MCHC) is a crucial blood test, but sometimes, other factors like ADHD, or attention deficit hyperactivity disorder, can impact overall health, affecting things like red blood cell production. Understanding the definition, symptoms, traits, causes, and treatment options for ADHD is key to comprehensive well-being. For a deeper dive into this complex condition, check out this informative resource: adhd attention deficit hyperactivity disorder included definition symptoms traits causes treatment.
Ultimately, MCHC provides a valuable piece of the puzzle in assessing red blood cell health.
Table of MCHC, MCV, MCH, and Normal Ranges
| Parameter | Normal Range | Abnormal Result (Example) | Possible Diagnoses |
|---|---|---|---|
| MCHC | 32-36 g/dL | 28 g/dL | Iron deficiency anemia, thalassemia |
| MCV | 80-100 fL | 70 fL | Microcytic anemia |
| MCH | 27-32 pg | 20 pg | Iron deficiency anemia |
The table above provides a general overview of normal ranges and examples of abnormal results for MCHC, MCV, and MCH. It’s crucial to note that these are just examples, and a definitive diagnosis requires a comprehensive evaluation by a healthcare professional, considering various factors beyond these indices.
Mean corpuscular hemoglobin concentration (MCHC) is a blood test that measures the average concentration of hemoglobin within red blood cells. Recently, the news about the Coca-Cola Zero Sugar Lemonade recall here got me thinking about potential health implications. While the recall likely doesn’t directly impact MCHC, it highlights the importance of carefully scrutinizing ingredients in our drinks, especially for those with existing blood-related conditions.
Understanding MCHC levels is crucial for diagnosing and managing various health concerns.
Measurement and Methodology
Mean Corpuscular Hemoglobin Concentration (MCHC) is a crucial hematological parameter reflecting the average concentration of hemoglobin within a single red blood cell. Accurate measurement is vital for diagnosing various anemias and other blood disorders. Understanding the methods used, the steps involved, and the potential sources of error in MCHC measurements is essential for clinicians and laboratory personnel.
Methods of MCHC Measurement
Different methods exist for measuring MCHC in a clinical laboratory. These methods vary in their principles, instrumentation, and overall cost. Choosing the appropriate method depends on the specific needs of the laboratory, including its resources, throughput requirements, and desired accuracy.
Spectrophotometry
Spectrophotometry is a widely used method for MCHC determination. This method relies on the principle of measuring the absorbance of light by a sample of whole blood. The absorbance is directly related to the concentration of hemoglobin within the blood sample. The measurement process involves the following steps:
- A blood sample is prepared by hemolysing the red blood cells, releasing hemoglobin into the solution.
- The concentration of hemoglobin in the resulting solution is measured using a spectrophotometer.
- The MCHC value is calculated by dividing the hemoglobin concentration by the hematocrit.
This method is relatively straightforward, cost-effective, and widely available in many clinical laboratories. However, the accuracy and precision can be affected by factors such as the quality of the reagents used and the technique of sample preparation.
Automated Hematology Analyzers
Automated hematology analyzers are increasingly prevalent in modern clinical laboratories. These instruments provide a comprehensive suite of hematological parameters, including MCHC. The method employed within these analyzers typically involves:
- The blood sample is processed through the instrument, which automatically separates the components of blood.
- The instrument measures the hemoglobin concentration and hematocrit using advanced optical techniques.
- The instrument calculates MCHC from the measured values.
Automated methods offer high throughput, speed, and precision. They are less susceptible to human error compared to manual spectrophotometric methods. However, the initial cost of these instruments can be a significant investment.
Limitations and Sources of Error
Several factors can affect the accuracy and precision of MCHC measurements. These include:
- Improper Sample Handling: Errors in blood collection, handling, and storage can lead to inaccurate results. Improper anticoagulation or hemolysis can affect the final result.
- Reagent Quality: The quality of the reagents used in the measurement process can influence the accuracy of the results. Contamination or expiration of reagents can introduce errors.
- Instrument Calibration: Regular calibration of the spectrophotometer or automated analyzer is crucial to maintain accuracy. Malfunctioning instruments can produce inaccurate measurements.
- Technical Errors: Errors in the procedures followed during sample preparation or measurement can also contribute to inaccuracies.
Comparison of Methods
| Method | Accuracy | Precision | Cost |
|---|---|---|---|
| Spectrophotometry | Moderate | Moderate | Low |
| Automated Hematology Analyzers | High | High | High |
The table above provides a general comparison of the different methods. The specific values for accuracy, precision, and cost can vary depending on the particular instrument and laboratory. Factors such as instrument maintenance and the expertise of the laboratory personnel can significantly influence the outcomes.
Interpretation of Results
Mean Corpuscular Hemoglobin Concentration (MCHC) provides crucial insights into the red blood cell’s hemoglobin content. Understanding its normal range, elevated values, and decreased values helps clinicians assess various conditions affecting red blood cell function. Correct interpretation of MCHC is vital in diagnosing and managing anemia and other related disorders.
Normal Range
The normal range for MCHC in healthy adults typically falls between 32-36 g/dL. Variations can exist based on age, sex, and other factors, but this range is generally accepted as indicative of healthy red blood cell function. Deviation from this range can suggest underlying conditions.
Elevated MCHC Values
Elevated MCHC values, exceeding the upper limit of the normal range, often indicate conditions characterized by increased hemoglobin concentration within red blood cells. This can occur in certain types of dehydration, or in conditions where there is an increased rate of red blood cell production or concentration. In these cases, the body compensates by concentrating hemoglobin in the existing red blood cells to maintain adequate oxygen-carrying capacity.
Decreased MCHC Values
Decreased MCHC values, falling below the lower limit of the normal range, typically suggest conditions where the red blood cells contain less hemoglobin than normal. This is often seen in anemias, where the body struggles to produce enough healthy red blood cells or hemoglobin. Examples include iron deficiency anemia, thalassemia, and certain chronic diseases. This reduction can lead to decreased oxygen delivery to the tissues.
MCHC in Conjunction with Other Parameters
Interpreting MCHC values in isolation is insufficient. Clinicians use MCHC in conjunction with other hematological parameters like red blood cell count (RBC), mean corpuscular volume (MCV), and mean corpuscular hemoglobin (MCH) to form a comprehensive picture of the patient’s blood condition. These parameters, when evaluated together, offer a more accurate diagnosis. For example, a low MCHC combined with a low MCV might suggest iron deficiency anemia, whereas a low MCHC with a high MCV might point towards other forms of anemia.
Clinical Interpretation Table
| MCHC Value (g/dL) | Clinical Interpretation | Possible Underlying Conditions |
|---|---|---|
| >36 | Elevated MCHC; possible dehydration, increased red blood cell production, or concentration. | Dehydration, polycythemia vera, certain types of chronic kidney disease. |
| 32-36 | Normal MCHC; indicative of healthy red blood cell function. | Healthy individuals. |
| <32 | Decreased MCHC; often associated with various anemias. | Iron deficiency anemia, thalassemia, sickle cell anemia, chronic diseases, lead poisoning. |
Clinical Applications
Mean Corpuscular Hemoglobin Concentration (MCHC) serves as a valuable diagnostic tool in hematology, offering insights into red blood cell health and function. Understanding how MCHC relates to various conditions allows clinicians to make informed decisions about diagnosis and treatment. Its significance extends from identifying anemia to monitoring the progression of hematological disorders and evaluating treatment efficacy.
MCHC in Anemia Diagnosis
MCHC plays a crucial role in diagnosing different types of anemia. By evaluating the concentration of hemoglobin within red blood cells, MCHC provides a quantitative assessment of the hemoglobin content per unit volume of red blood cells. Variations in MCHC can pinpoint the underlying cause of anemia, guiding treatment strategies. For example, a low MCHC often suggests a deficiency in hemoglobin production or a loss of red blood cells, whereas a high MCHC might indicate a different underlying cause, such as dehydration or certain blood disorders.
Types of Anemia and Their Effect on MCHC
Different types of anemia exhibit distinct MCHC patterns. For instance, iron deficiency anemia, a common type of anemia, typically results in a low MCHC due to inadequate hemoglobin synthesis. Similarly, thalassemia, a group of inherited blood disorders, frequently shows a low MCHC. These disorders disrupt the production of the hemoglobin molecule, which directly affects the MCHC. In contrast, spherocytosis, a hereditary condition causing red blood cells to become spherical and fragile, often results in a high MCHC.
This is because the reduced cell volume concentrates the hemoglobin within the smaller cells.
MCHC and Hemolytic Conditions
Hemolytic conditions, characterized by the premature destruction of red blood cells, can be identified using MCHC. A low MCHC, combined with other clinical findings, may indicate hemolysis. This is because the rapid destruction of red blood cells leads to a loss of hemoglobin and a decreased MCHC. The presence of fragmented red blood cells (schistocytes) on a blood smear, along with a low MCHC, strongly suggests a hemolytic process.
Monitoring Treatment Effectiveness
MCHC measurements can track the effectiveness of treatments for hematological disorders. For example, in iron deficiency anemia, increasing iron intake should lead to an improvement in hemoglobin synthesis, reflected by a rising MCHC. Similarly, monitoring MCHC during treatment for thalassemia can provide insights into the response to therapies aimed at managing the disease.
MCHC and Disease Progression
MCHC can help monitor the progression of certain diseases. In chronic kidney disease, for example, the decline in red blood cell production and hemoglobin synthesis often results in a decreasing MCHC. Careful monitoring of MCHC can assist in evaluating the progression of the disease and the need for interventions.
Table of Anemia Types and MCHC Values
| Type of Anemia | Characteristic MCHC Value | Explanation |
|---|---|---|
| Iron Deficiency Anemia | Low | Insufficient iron impairs hemoglobin production. |
| Thalassemia | Low | Defects in hemoglobin synthesis reduce hemoglobin levels. |
| Spherocytosis | High | Smaller red blood cell volume concentrates hemoglobin. |
| Aplastic Anemia | Variable, often low | Bone marrow failure leads to reduced red blood cell production. |
| Sickle Cell Anemia | Variable, often low | Abnormal hemoglobin causes red blood cell deformation and destruction. |
Variations and Factors Affecting MCHC
Mean Corpuscular Hemoglobin Concentration (MCHC) provides valuable insights into red blood cell health. However, MCHC values aren’t static; they can fluctuate based on a multitude of factors. Understanding these variations is crucial for accurate interpretation and effective patient management. This section delves into the influences on MCHC, exploring disease impacts, nutritional connections, and the role of demographic factors.
Factors Influencing MCHC Levels
MCHC is affected by various internal and external factors. These factors include underlying diseases, nutritional deficiencies, and even demographic characteristics like age and gender. The interplay of these elements contributes to the variability seen in MCHC values.
Effect of Diseases on MCHC
Several diseases can significantly impact MCHC levels. For instance, hemolytic anemias, characterized by the premature destruction of red blood cells, often lead to decreased MCHC. Conversely, conditions that affect hemoglobin synthesis, like iron deficiency anemia, can result in lower MCHC values. Similarly, certain chronic diseases can influence MCHC, though the relationship may be complex and dependent on the specific disease.
For example, chronic kidney disease may lead to altered MCHC, potentially impacting the synthesis of red blood cells.
Influence of Age, Gender, and Ethnicity on MCHC, Mean corpuscular hemoglobin concentration
Age, gender, and ethnicity can also play a role in MCHC values. While generally, these factors have less significant impacts on MCHC compared to diseases and nutritional status, subtle variations might be observed in specific populations. For instance, some studies suggest subtle differences in MCHC levels across different ethnic groups, potentially linked to genetic predispositions.
Nutritional Deficiencies and MCHC
Nutritional deficiencies, particularly iron deficiency, are strong contributors to lower MCHC values. Iron is essential for hemoglobin production. A lack of iron directly impacts the amount of hemoglobin in red blood cells, thus lowering the MCHC. Other nutritional deficiencies, such as deficiencies in vitamin B12 or folate, can also indirectly affect MCHC by impacting red blood cell production and maturation.
Table of Factors Affecting MCHC
| Factor | Potential Impact on MCHC |
|---|---|
| Hemolytic Anemias | Decreased MCHC |
| Iron Deficiency Anemia | Decreased MCHC |
| Chronic Kidney Disease | Potentially decreased or increased MCHC (depending on the specific case) |
| Vitamin B12 Deficiency | Decreased MCHC (indirectly) |
| Folate Deficiency | Decreased MCHC (indirectly) |
| Age | Potentially subtle variations |
| Gender | Potentially subtle variations |
| Ethnicity | Potentially subtle variations |
Visual Representation and Illustrations
Visual representations are crucial for understanding complex concepts like MCHC. Graphs and diagrams can translate numerical data into easily digestible forms, allowing for quicker comprehension and identification of trends or patterns. These visual aids significantly enhance the learning process and facilitate the interpretation of MCHC data in clinical settings.
MCHC Distribution Curve in a Healthy Population
A healthy population’s MCHC distribution follows a roughly bell-shaped curve, centered around a specific mean value. The majority of individuals fall within a relatively narrow range around this average, indicating a normal range for MCHC. The curve’s width reflects the variability within the healthy population, showcasing the natural distribution of MCHC values. This distribution provides a baseline for comparison and helps clinicians quickly assess whether an individual’s MCHC falls outside the expected range.
Relationship Between MCHC and Other Red Blood Cell Indices
The relationship between MCHC and other red blood cell indices like MCV and MCH can be visualized using a scatter plot. The x-axis would represent MCV, the y-axis MCH, and each data point would represent an individual’s MCHC value. A positive correlation would be apparent, with higher MCHC values generally aligning with higher MCV and MCH values. This correlation illustrates the interconnectedness of these indices in reflecting the overall health of red blood cells.
Deviation from this typical pattern could suggest underlying hematological issues.
Impact of Different Types of Anemia on MCHC
Different types of anemia affect MCHC in distinct ways, which can be illustrated using separate scatter plots or grouped bar graphs. For instance, iron deficiency anemia, characterized by low iron levels, would typically manifest with a lower MCHC. Similarly, thalassemias, a group of genetic disorders, might exhibit lower or even normal MCHC, depending on the specific type. Hemolytic anemias, where red blood cells are destroyed prematurely, could display variable MCHC depending on the underlying cause and the rate of red blood cell destruction.
The visual comparison would highlight the distinct patterns of MCHC changes associated with various anemic conditions.
MCHC Changes Over Time During Treatment
Visualizing MCHC changes over time during treatment for a hematological condition is best illustrated using a line graph. The x-axis would represent time (e.g., weeks or months), and the y-axis would represent MCHC values. The graph would show the progression of MCHC levels during the treatment period. For example, in iron deficiency anemia, a gradual increase in MCHC over time, as iron supplementation is administered, would be observed.
A similar visualization could be applied to other hematological conditions, such as sickle cell disease or aplastic anemia, to monitor treatment efficacy.
Epilogue: Mean Corpuscular Hemoglobin Concentration
In conclusion, mean corpuscular hemoglobin concentration (MCHC) serves as a cornerstone in hematological assessments. Its measurement and interpretation provide invaluable insights into red blood cell health and the potential presence of underlying conditions like anemia or hemolytic disorders. This comprehensive overview has highlighted the significance of MCHC in diagnostics and monitoring, underscoring its critical role in patient care.










