Ted Danson Plaque Psoriasis Awareness A Deeper Look
Ted Danson plaque psoriasis awareness highlights the importance of public figures using their platform to raise awareness about health issues....







Ted Danson plaque psoriasis awareness highlights the importance of public figures using their platform to raise awareness about health issues....
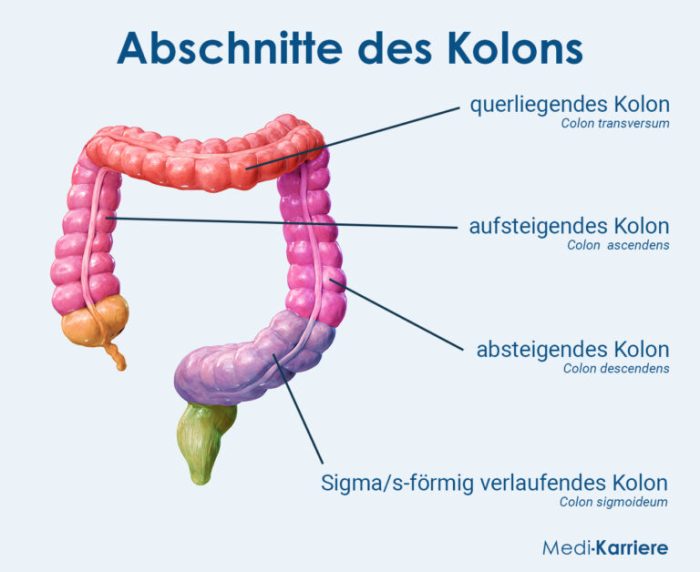
Panniculitis causes symptoms treatments and more, delving into the complexities of this inflammatory condition affecting the fat tissue beneath the...
Understanding hangover headaches and how to avoid them is crucial for anyone who enjoys social gatherings or occasional celebrations involving...
Eye allergies in kids can be a real pain, impacting their comfort and well-being. From itchy, watery eyes to frustrating...
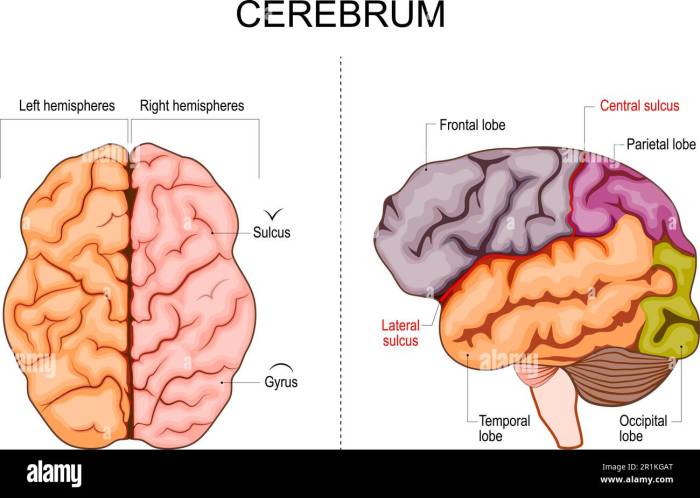
Progesterone and brain health is a fascinating area of study. This exploration delves into the intricate relationship between progesterone, a...
Sunflower pumpkin sesame seeds – a powerhouse trio of nutritional gems! From their diverse culinary applications to their profound health...
The differences between Saxenda and Wegovy are key for anyone considering these weight management medications. Both are GLP-1 receptor agonists,...
Enterovirus strains and facts cover a wide range of topics, from the basics of what enteroviruses are to their impact...
Rapid onset gender dysphoria is a complex and often misunderstood condition. It’s characterized by a sudden and significant shift in...
How to stop night gout pain at night is a crucial question for those suffering from this agonizing condition. This...