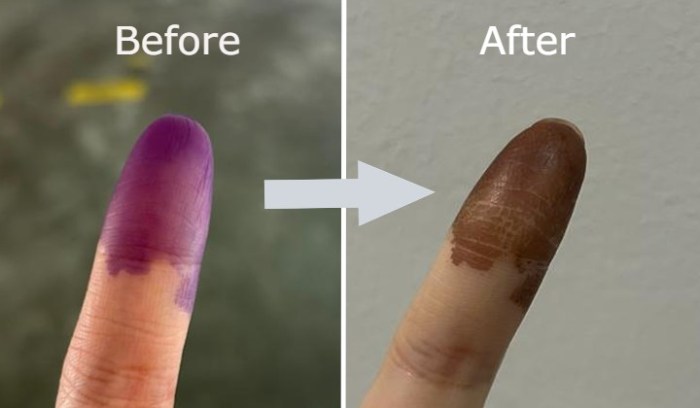
What causes a purple finger? This seemingly simple question delves into a complex interplay of medical conditions, circulatory issues, infections, trauma, and even lifestyle choices. Understanding the underlying causes is crucial for effective diagnosis and treatment, ensuring a swift return to health and well-being.
From vascular disorders to infections, a range of factors can contribute to this unsettling discoloration. This exploration will uncover the mechanisms behind these conditions, highlighting the symptoms, risk factors, and potential treatments.
Possible Medical Causes
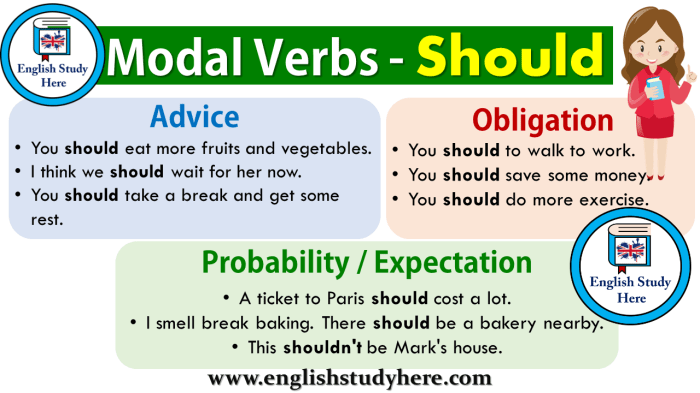
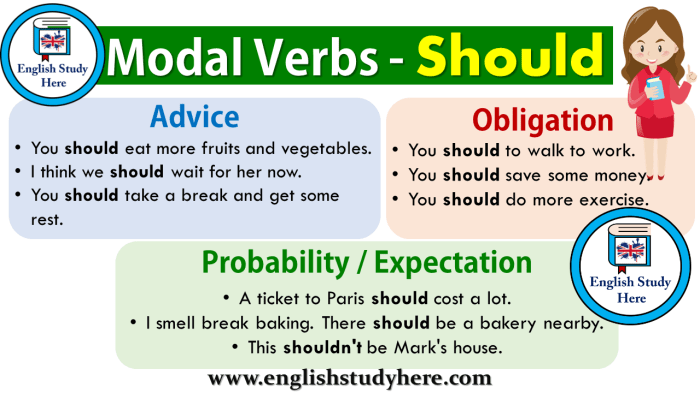
A purple finger, or a finger exhibiting cyanosis, can be a concerning symptom, potentially indicating an underlying medical condition. Understanding the potential causes and their associated symptoms is crucial for prompt diagnosis and appropriate treatment. This section will delve into various medical conditions that can manifest as purple discoloration in the fingers, examining their mechanisms, accompanying symptoms, and variations in presentation.
Vascular Disorders
Vascular disorders significantly impact blood flow, often leading to reduced oxygenation and the characteristic purple hue. These conditions can range from relatively benign to life-threatening. Several conditions disrupt normal blood flow, potentially causing a purple finger.
- Raynaud’s Phenomenon: This condition causes episodic vasospasm, or narrowing of the blood vessels in the extremities, particularly in response to cold temperatures or stress. Reduced blood flow to the fingers leads to the characteristic blanching (pallor), followed by cyanosis (purple discoloration), and eventually redness as blood flow returns. Symptoms often include numbness, tingling, and pain in addition to the color changes.
Severity can vary; some individuals experience mild episodes, while others have more frequent and intense attacks. For instance, a person might experience a purple fingertip during a particularly cold winter day or after prolonged exposure to a very cold environment.
- Peripheral Arterial Disease (PAD): PAD is a narrowing of the arteries in the extremities, often due to atherosclerosis. This condition reduces blood flow to the limbs, leading to a range of symptoms, including intermittent claudication (pain with exercise), numbness, and coolness in the affected extremities. The purple discoloration can be a more severe sign, indicative of advanced stages of PAD. A person with PAD may experience a noticeably purple finger, especially during periods of reduced blood flow.
For instance, someone with PAD might experience a purple finger while walking uphill or performing other strenuous activities.
- Buerger’s Disease (Thromboangiitis Obliterans): This rare condition involves inflammation and narrowing of the arteries and veins, particularly in the extremities. It often affects smokers and presents with pain, swelling, and a bluish-purple discoloration of the fingers and toes. Symptoms can be severe and progressive, potentially leading to tissue damage and amputation. The discoloration in Buerger’s Disease can be quite pronounced and may not respond to conventional treatments as quickly as other conditions.
Autoimmune Diseases
Autoimmune diseases can affect blood vessels, leading to inflammation and impaired circulation, manifesting as a purple finger. These conditions are characterized by an overactive immune system that attacks healthy tissues.
- Systemic Lupus Erythematosus (SLE): SLE is a chronic autoimmune disease that can affect various organs and systems. It often involves inflammation of the blood vessels, leading to symptoms like purple discoloration, particularly in the fingers and other extremities. This discoloration can be accompanied by other lupus-related symptoms such as joint pain, fatigue, and skin rashes. The severity of the purple discoloration can vary, and in some cases, it might be subtle and not immediately noticeable.
A patient with SLE may experience a slight purple tinge in the fingers, which could be more pronounced during periods of exacerbation.
- Scleroderma: Scleroderma is an autoimmune disease characterized by the hardening and thickening of the skin and connective tissues. This condition can affect blood vessels, leading to impaired circulation and potentially a purple discoloration in the fingers. The skin changes associated with scleroderma can also manifest as stiffness, tightness, and reduced mobility. The purple color might be accompanied by skin tightening and firmness in the affected areas.
Infections
Infections can also cause a purple finger through various mechanisms, including inflammation and impaired blood flow.
A purple finger, often a sign of poor circulation, can be caused by a number of things, from cold exposure to underlying health conditions. While exploring the various causes, it’s interesting to note how some of the same principles that improve circulation might also be helpful for weight management, such as using peptides for weight loss. Peptides for weight loss are often touted as a way to boost metabolism and potentially improve overall health, but remember that a purple finger is still a sign to check with your doctor to rule out more serious conditions.
Ultimately, proper diagnosis and treatment are key.
- Cellulitis: Cellulitis is a bacterial infection of the skin and underlying tissues. It can cause inflammation, redness, swelling, and a warm sensation in the affected area, potentially leading to a purple discoloration, particularly if the infection is severe. The purple discoloration may be accompanied by fever, chills, and other systemic symptoms.
Comparative Analysis of Conditions
| Condition | Symptoms | Risk Factors | Treatment |
|---|---|---|---|
| Raynaud’s Phenomenon | Color changes (white, blue, red), numbness, tingling, pain | Cold temperatures, stress, smoking | Lifestyle modifications (avoiding cold, stress reduction), medications |
| Peripheral Arterial Disease (PAD) | Intermittent claudication, numbness, coolness, potential for purple discoloration | Smoking, high blood pressure, high cholesterol, diabetes | Lifestyle modifications, medications (antiplatelet agents), potential for surgical interventions |
| Buerger’s Disease | Pain, swelling, bluish-purple discoloration, potential for tissue damage | Smoking | Smoking cessation, medications, potential for surgical interventions |
| Systemic Lupus Erythematosus (SLE) | Joint pain, fatigue, skin rashes, purple discoloration | Genetic predisposition, environmental factors | Medications (immunosuppressants), management of symptoms |
| Scleroderma | Skin hardening, tightening, reduced mobility, potential for purple discoloration | Genetic predisposition, environmental factors | Medications (immunosuppressants), management of symptoms |
| Cellulitis | Redness, swelling, warmth, potential for purple discoloration | Open wounds, weakened immune system | Antibiotics, wound care |
Circulatory Issues
Healthy blood circulation is crucial for maintaining the vibrant hues of our fingers, as well as the overall health of our extremities. Proper blood flow delivers oxygen and nutrients, contributing to the pinkish tone of our skin. Poor circulation, on the other hand, can lead to a range of issues, impacting not just the appearance but also the functionality of our fingers.
The Role of Blood Circulation in Finger Color
Blood vessels in the fingers carry oxygenated blood, giving the skin its characteristic color. Changes in blood flow, whether due to reduced blood supply or altered blood composition, can manifest as discoloration. Adequate blood flow is essential for maintaining the healthy, pinkish hue of the fingertips. A decrease in blood flow can lead to a pale, bluish, or even purplish appearance, depending on the underlying cause.
Disruptions to Normal Blood Flow
Several factors can disrupt the normal flow of blood to the fingers, leading to circulatory issues. These disruptions can stem from various conditions, including:
- Narrowed or blocked arteries: Conditions like atherosclerosis, where plaque builds up in the arteries, can restrict blood flow. This can result in reduced oxygen and nutrient delivery to the fingers, potentially leading to discoloration. Smoking, high cholesterol, and high blood pressure are significant risk factors for atherosclerosis. For example, a patient with severe atherosclerosis may experience intermittent claudication, a pain in the legs and feet, and a bluish tinge in the affected extremities during exercise.
- Reduced blood volume: Severe dehydration or blood loss can decrease the overall blood volume, leading to decreased blood flow to the extremities, including the fingers. This reduction in blood flow can lead to a pale appearance in the fingers.
- Damage to blood vessels: Injury or trauma to blood vessels can cause inflammation and blockage, impeding blood flow. Frostbite, for example, can damage small blood vessels, leading to a bluish-purple discoloration in the affected area.
Comparison of Circulatory Disorders
Various circulatory disorders can impact finger color differently. Peripheral artery disease (PAD) is characterized by the narrowing of arteries, reducing blood flow to the extremities. Raynaud’s phenomenon, on the other hand, involves spasms in the blood vessels, leading to temporary constriction and discoloration. While both can cause changes in finger color, the mechanisms and underlying causes differ significantly.
Impact of Lifestyle Factors
Lifestyle choices play a significant role in maintaining healthy circulation. A diet high in saturated fats and cholesterol contributes to plaque buildup in arteries. Lack of physical activity can weaken the cardiovascular system, potentially affecting blood flow. Smoking significantly damages blood vessels, making them more susceptible to blockage and reducing overall blood flow. These factors contribute to a higher risk of developing circulatory disorders.
Table of Circulatory Disorders
| Disorder | Symptoms | Diagnosis | Treatment |
|---|---|---|---|
| Peripheral Artery Disease (PAD) | Pain, numbness, tingling, cramping in legs and feet, especially during exercise; cool or pale skin; weak or absent pulses; hair loss on legs; sores that don’t heal | Physical exam, ankle-brachial index (ABI) test, Doppler ultrasound, angiography | Lifestyle modifications (diet, exercise, smoking cessation), medication (antiplatelet drugs, statins), surgical interventions (angioplasty, bypass surgery) |
| Raynaud’s Phenomenon | Color changes in fingers and toes (white, blue, red) in response to cold or stress; numbness, tingling, pain | Physical exam, medical history, observation of color changes | Lifestyle modifications (avoiding cold, stress reduction), medication (calcium channel blockers), other therapies |
| Venous Insufficiency | Swelling, aching, heaviness in legs; skin changes (thickening, discoloration, ulcers); varicose veins | Physical exam, ultrasound, venous duplex scan | Compression stockings, elevation, exercise, medication, surgery |
Diagnostic Procedures
Diagnosing circulatory issues involves a combination of methods, including a physical examination, medical history review, and specific tests. A physical exam allows the physician to assess for signs like reduced pulses, skin discoloration, and swelling. Further tests such as the ankle-brachial index (ABI) and Doppler ultrasound can provide more specific information about blood flow in the extremities. Angiography, a more advanced technique, allows visualization of the arteries and veins.
Infections and Inflammatory Conditions

Purple fingers can sometimes be a sign of an underlying infection or inflammatory process. These conditions can cause inflammation, which can lead to changes in blood flow and ultimately, the characteristic discoloration. Understanding these mechanisms is crucial for accurate diagnosis and effective treatment.
How Infections Affect Blood Vessels
Infections, whether bacterial, viral, or fungal, can trigger an inflammatory response in the body. This response, while vital for fighting off the infection, can also have unintended consequences. Inflammation involves the release of various chemicals and proteins, which can cause the blood vessels in the affected area to become inflamed, leaky, and constricted. This can lead to a reduction in blood flow, potentially causing the fingers to appear purple.
In some cases, the inflammation can directly damage the blood vessels, further disrupting blood flow and contributing to discoloration.
Infectious Agents Causing Inflammation and Discoloration
Several infectious agents can cause inflammation and result in purple fingers. These include bacteria like Streptococcus pyogenes (responsible for strep throat), Staphylococcus aureus (a common skin infection culprit), and various other bacterial species. Viral infections, such as certain types of influenza or even some forms of COVID-19, can also trigger inflammation and discoloration in the extremities. Fungal infections, although less common in causing this symptom, can still be a factor, particularly in individuals with compromised immune systems.
Ever wondered what causes a purple finger? It could be a number of things, from circulation issues to a reaction to something you touched. Sometimes, it’s just a temporary issue, but if it persists, it’s always a good idea to see a doctor. On a completely different note, if you’re dealing with an annoying eye twitch, learning how to stop it could be just what you need.
For a comprehensive guide on how to stop an eye twitch, check out this helpful article how to stop an eye twitch. Regardless of the cause, if your finger stays purple for a while, it’s always wise to seek professional medical advice. This will help determine the underlying reason and suggest the right course of action.
Role of Inflammation in Altering Finger Color, What causes a purple finger
Inflammation is a complex biological response to harmful stimuli. Key to understanding its effect on finger color is the interplay of blood vessels, blood flow, and the release of inflammatory mediators. These mediators, such as histamine and cytokines, cause the blood vessels to dilate or constrict, and become more permeable. This alteration in blood flow, combined with the pooling of blood in the affected area, contributes to the purple hue.
Furthermore, inflammation can also lead to the formation of blood clots, which further restrict blood flow and worsen the discoloration.
Inflammatory Conditions Causing Purple Fingers
Several inflammatory conditions can manifest as purple fingers, reflecting the impact of the inflammation on blood flow and vessel integrity. These conditions are often accompanied by other symptoms, and accurate diagnosis is essential for appropriate treatment.
- Cellulitis: A bacterial skin infection characterized by redness, swelling, warmth, and pain. The infection can spread quickly, and prompt treatment is crucial to prevent complications.
- Rheumatoid Arthritis: An autoimmune disorder that affects the joints. In some cases, rheumatoid arthritis can affect the blood vessels, leading to inflammation and discoloration in the extremities. The progression can vary, with some individuals experiencing symptoms only occasionally, while others have more consistent and severe symptoms.
- Vasculitis: A condition involving inflammation of the blood vessels. Various types of vasculitis exist, each with its own set of symptoms and potential complications. Vasculitis can manifest with varying degrees of severity, affecting different parts of the body, and sometimes leading to significant organ damage.
- Raynaud’s phenomenon: While not an infection, this condition can cause discoloration, including purple, in the fingers due to spasms of the blood vessels in response to cold or stress. This condition, often triggered by cold exposure, can be a significant cause of purple discoloration.
Diagnosis of Infections and Inflammatory Conditions
Diagnosing infections and inflammatory conditions responsible for purple fingers requires a thorough evaluation. Physical examination, including assessment of the affected area, is a crucial first step. Further diagnostic procedures may include blood tests to detect inflammatory markers, such as C-reactive protein (CRP), or specific markers for infections. Imaging studies, like X-rays or ultrasounds, can reveal underlying structural abnormalities or signs of inflammation.
A biopsy of the affected tissue might be necessary in certain cases, particularly when the cause is unclear.
| Infection/Condition | Symptoms | Diagnosis | Treatment |
|---|---|---|---|
| Cellulitis | Redness, swelling, warmth, pain, fever | Physical examination, blood tests (CRP), imaging (ultrasound) | Antibiotics, pain management |
| Rheumatoid Arthritis | Joint pain, stiffness, swelling, fatigue | Physical examination, blood tests (rheumatoid factor), imaging (X-rays) | Disease-modifying antirheumatic drugs (DMARDs), pain relief |
| Vasculitis | Systemic symptoms, including fever, fatigue, muscle aches, skin lesions | Physical examination, blood tests (inflammatory markers, blood count), biopsy, imaging (biopsy) | Corticosteroids, immunosuppressants |
| Raynaud’s phenomenon | Color changes (white, blue, purple) in fingers or toes, numbness, tingling | Physical examination, blood tests (if other conditions are suspected) | Lifestyle changes (avoiding cold exposure), medications (in severe cases) |
Trauma and Injuries
Trauma to the fingers, ranging from minor cuts to severe fractures, can significantly impact blood flow and lead to discoloration, often appearing as a purplish hue. Understanding the different types of injuries and their effects on circulation is crucial for appropriate diagnosis and treatment. The severity of the injury directly correlates with the intensity of the discoloration, as more severe damage restricts blood flow more significantly.Injuries to the fingers can stem from various sources, including accidents, falls, sports-related incidents, or even repetitive stress.
These injuries can lead to a range of issues, including broken bones, lacerations, and contusions, each impacting the circulatory system in its own way. Prompt medical attention is essential for effective treatment and minimizing potential long-term complications.
Types of Injuries and Their Effects
Injuries to the fingers can range from minor to severe, impacting the circulatory system in various ways. Different types of trauma can have varying degrees of impact on blood flow, affecting the appearance and potential complications.
- Fractures: Broken bones, whether simple or complex, can disrupt blood vessels and impair circulation. The extent of the disruption depends on the fracture’s location and severity. For example, a simple hairline fracture might cause minimal discoloration, whereas a comminuted fracture (bone splintered into many pieces) could lead to significant discoloration and swelling. Proper alignment and stabilization of the fractured bone are crucial for restoring normal blood flow and preventing long-term problems.
- Lacerations: Cuts and tears in the skin can compromise blood vessels, leading to bleeding and discoloration. Deep lacerations, especially those involving tendons or nerves, may result in more severe and prolonged discoloration due to extensive blood loss and potential nerve damage. Treatment focuses on controlling bleeding, cleaning the wound, and potentially stitching it to restore normal blood flow.
- Contusions (Bruises): Blunt force trauma to the fingers can cause bleeding within the tissues, resulting in a purplish discoloration. The severity of the bruise, determined by the force and duration of the impact, dictates the extent of the discoloration and potential for complications like compartment syndrome. Treatment generally involves rest, ice, compression, and elevation (RICE).
- Amputations: In cases of severe trauma, an amputation might be necessary. This directly impacts the blood supply to the affected area, leading to immediate and significant discoloration, and potential long-term complications depending on the extent of the loss and the patient’s health.
Severity and Discoloration
The severity of the injury plays a crucial role in determining the intensity of the discoloration. A minor contusion might result in a subtle purplish or bluish discoloration, whereas a severe fracture or laceration can cause a more pronounced and extensive discoloration. The degree of discoloration is not always a definitive indicator of the severity of the injury, but it often provides a visual clue to the extent of the damage.
Treatment Procedures
Prompt medical attention is essential for any injury causing purple fingers. Treatment varies based on the type and severity of the injury. Common procedures may include:
- First Aid: Immediate first aid, such as applying pressure to stop bleeding, is crucial. This can help minimize blood loss and the intensity of discoloration.
- Immobilization: For fractures, immobilization using splints or casts is necessary to maintain alignment and prevent further damage.
- Surgical Intervention: In cases of severe lacerations, fractures, or amputations, surgical intervention might be necessary to repair the damage and restore blood flow.
- Medications: Pain relievers and anti-inflammatory medications may be prescribed to manage pain and swelling.
- Physical Therapy: Post-injury rehabilitation may involve physical therapy to restore function and mobility.
Potential Long-Term Effects
The long-term effects of injuries to the fingers can vary significantly depending on the type, severity, and the individual’s response to treatment. Possible complications include:
- Chronic Pain: Persistent pain may result from nerve damage or other complications.
- Limited Range of Motion: Scar tissue formation or joint damage can restrict movement.
- Circulatory Problems: In severe cases, the injury can lead to long-term circulatory issues.
- Infection: Open wounds increase the risk of infection.
Comparison of Injury Types
| Injury Type | Symptoms | Treatment | Potential Complications |
|---|---|---|---|
| Fractures | Pain, swelling, deformity, bruising, impaired movement | Immobilization, pain relief, potentially surgery | Delayed healing, malunion, nonunion, compartment syndrome |
| Lacerations | Bleeding, pain, visible cuts or tears | Cleaning, sutures, wound care | Infection, scarring, nerve damage |
| Contusions | Pain, swelling, bruising (purple or bluish discoloration) | RICE (rest, ice, compression, elevation) | Compartment syndrome, delayed healing |
Lifestyle Factors: What Causes A Purple Finger
Our lifestyle choices play a significant role in our overall health, including the health of our circulatory system. Factors like diet, exercise, and habits like smoking can influence blood flow and contribute to conditions that manifest as purple fingers. Understanding these influences is crucial for proactive health management.Lifestyle factors can significantly impact blood circulation, potentially leading to discoloration or other issues in the extremities like fingers.
Prolonged exposure to cold temperatures, for instance, can constrict blood vessels, while habits like smoking can damage the delicate lining of blood vessels. These factors, along with other lifestyle choices, can contribute to a range of circulatory problems, including those that may cause purple fingers.
Prolonged Exposure to Cold Temperatures
Exposure to prolonged and intense cold can constrict blood vessels, reducing blood flow to the extremities like fingers and toes. This is a common physiological response to cold, designed to conserve heat in the core of the body. However, repeated or prolonged exposure can lead to impaired circulation and potential damage to tissues. Individuals living in colder climates or frequently engaging in cold-water activities might experience this effect more acutely.
For example, a person who frequently participates in winter sports without proper protective gear may develop cold-induced changes in their extremities, including a bluish or purplish discoloration.
Effects of Smoking and Other Habits on Blood Vessels
Smoking is a significant risk factor for vascular damage. The chemicals in cigarettes can damage the lining of blood vessels (endothelium), leading to inflammation and narrowing of the arteries. This reduces blood flow and can increase the risk of various circulatory problems, including those that could cause purple fingers. Other habits like excessive alcohol consumption can also have a detrimental effect on blood vessels.
Ever wondered what causes a purple finger? It could be a few things, from a simple bruise to something more serious. Learning how to care for vulvar dermatitis symptoms and treatment methods can be surprisingly helpful in understanding some of the less obvious causes of discoloration. For instance, certain skin conditions can manifest as purple fingers, and understanding the proper care for these conditions is key.
If you’re looking for expert advice on how to care for vulvar dermatitis symptoms and treatment methods, check out this helpful guide: how to care for vulvar dermatitis symptoms and treatment methods. Ultimately, consulting a doctor is crucial for a proper diagnosis of any unusual discoloration, like a purple finger. It’s always best to get a professional opinion to rule out any underlying health issues.
Alcohol can lead to dehydration, which can affect blood viscosity and blood flow. Moreover, chronic alcohol abuse can damage the heart and blood vessels, contributing to overall circulatory issues.
Specific Lifestyle Choices Contributing to the Issue
Certain lifestyle choices can increase the risk of developing conditions that affect blood circulation. A diet lacking essential nutrients, such as vitamin C, vitamin E, and B vitamins, can compromise the health of blood vessels. A diet high in saturated fats and cholesterol can contribute to the build-up of plaque in arteries, further reducing blood flow. A sedentary lifestyle can also negatively affect circulation.
Lack of regular exercise can lead to sluggish blood flow, potentially impacting the health of the extremities.
Importance of Maintaining a Healthy Lifestyle for Overall Circulatory Health
Maintaining a healthy lifestyle is paramount for overall circulatory health. A balanced diet rich in fruits, vegetables, and whole grains, along with regular physical activity, can significantly improve blood flow and reduce the risk of circulatory problems. Quitting smoking and limiting alcohol consumption are also vital steps to promote healthy blood vessels. By adopting healthy habits, individuals can significantly improve their circulatory health and reduce the risk of developing conditions that may lead to purple fingers.
Lifestyle Recommendations to Minimize the Risk of Purple Fingers
- Adopt a balanced diet rich in fruits, vegetables, and whole grains, limiting saturated fats and cholesterol.
- Engage in regular physical activity to improve blood flow and overall cardiovascular health. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days a week.
- Avoid smoking and limit alcohol consumption. Smoking damages blood vessels and increases the risk of various circulatory issues. Limiting alcohol consumption to moderate levels is essential for overall health.
- Dress appropriately for cold temperatures, protecting extremities from prolonged exposure to extreme cold.
- Manage stress effectively, as stress can negatively impact blood circulation.
- Regular check-ups with a healthcare professional are crucial for early detection and management of any circulatory issues.
Illustrative Examples
Purple fingers, a condition often associated with discomfort and concern, can stem from a variety of underlying causes. Understanding the specific factors involved in each case is crucial for accurate diagnosis and effective treatment. This section provides illustrative examples to shed light on the diverse range of potential causes.
Case Study: Raynaud’s Phenomenon
Raynaud’s phenomenon is a condition characterized by intermittent episodes of reduced blood flow to the extremities, most notably the fingers and toes. During these episodes, the affected areas turn white, then blue, and finally purple, often accompanied by numbness and tingling. A patient experiencing Raynaud’s may describe a triggering event, such as exposure to cold temperatures or emotional stress.A 35-year-old female presented with a history of intermittent purple discoloration in her fingers, particularly during cold weather or periods of stress.
Her symptoms included numbness and a prickling sensation. Physical examination revealed a characteristic color change in the fingers upon exposure to cold. Diagnosis was confirmed through a combination of physical examination, patient history, and a blood test to rule out other conditions. Treatment focused on avoiding triggers like cold temperatures and stress, as well as using medication to improve blood circulation.
Regular monitoring and lifestyle modifications were essential for managing the condition effectively.
Specific Medical Condition: Acrocyanosis
Acrocyanosis is a benign condition characterized by a bluish or purplish discoloration of the hands and feet, particularly in the fingertips and toes. This discoloration is often more pronounced in cold environments or during periods of stress. The discoloration typically arises from an imbalance in blood flow to the extremities.
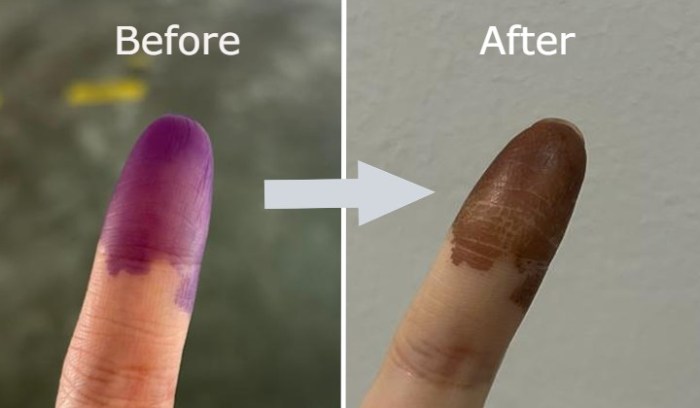
Injury or Trauma: Crush Injury
A crush injury to the hand or arm can cause significant disruption to blood vessels and nerves. The intense pressure exerted on the tissues can result in damaged blood vessels, leading to reduced blood flow and a purplish discoloration of the fingers. The severity of the injury will dictate the extent of the discoloration and the associated complications.
For instance, a severe crush injury might involve significant tissue damage, requiring extensive medical attention.
Lifestyle Choice: Smoking
Smoking is a significant risk factor for various circulatory issues. Nicotine in tobacco constricts blood vessels, reducing blood flow to the extremities. This vasoconstriction can lead to a bluish or purplish discoloration in the fingers, particularly in individuals who smoke heavily. The impact of smoking on circulation is well-documented, and individuals considering quitting smoking should consult with their healthcare provider.
Case Study: Combined Factors
A 65-year-old male with a history of diabetes and a recent episode of frostbite presented with persistent purple discoloration in his fingers. The patient also reported increased stress levels and a recent increase in smoking. The combination of pre-existing vascular issues (diabetes), trauma (frostbite), and lifestyle choices (smoking and stress) likely contributed to the persistent purple discoloration. Diagnosis and treatment involved addressing each contributing factor.
The management plan focused on improving blood circulation, controlling blood sugar, quitting smoking, and stress reduction techniques.
Closing Summary
In conclusion, the causes of purple fingers are multifaceted, encompassing medical conditions, circulatory problems, infections, trauma, and lifestyle factors. A thorough evaluation, considering these various aspects, is essential for accurate diagnosis and personalized treatment plans. Remembering that early intervention and appropriate medical care are key to restoring optimal health and well-being is crucial.