Foods high in magnesium are crucial for a healthy body. Magnesium plays a vital role in numerous bodily functions, from muscle contractions to nerve signals. A deficiency can lead to a range of problems, making it important to understand which foods are rich in this essential mineral. This guide delves into the world of magnesium-rich foods, exploring their nutritional value, health benefits, and practical dietary strategies for incorporating them into your daily routine.
This comprehensive exploration of magnesium-rich foods will cover everything from the importance of magnesium to a list of top sources, including vegetables, fruits, nuts, and seeds. We’ll also examine how preparation methods can impact magnesium levels, compare the magnesium content of various foods, and discuss potential interactions with other nutrients and medications.
Introduction to Magnesium
Magnesium is a crucial mineral that plays a vital role in numerous bodily functions. It’s involved in over 300 enzymatic reactions, acting as a co-factor for various processes, from muscle contractions to nerve impulses. Maintaining adequate magnesium levels is essential for overall health and well-being. A deficiency can lead to a range of symptoms and complications, highlighting the importance of including magnesium-rich foods in your diet.Magnesium is intricately linked to numerous physiological processes.
It’s essential for energy production, protein synthesis, and maintaining healthy blood sugar levels. It also plays a significant role in bone health and blood pressure regulation. Understanding the significance of magnesium in these processes underscores the importance of maintaining optimal magnesium levels.
Eating foods high in magnesium can be a great way to support overall health. However, if you’re noticing bright red blood in your stool, it’s crucial to seek professional medical advice. Checking out this resource on advice about bright red blood in stool can help you understand the potential causes and what steps to take. While magnesium-rich foods like spinach and almonds are generally healthy, it’s important to always consult a doctor before making significant dietary changes, especially if you have existing health conditions.
Importance of Magnesium in Bodily Functions
Magnesium is a fundamental component in various bodily processes. Its role in muscle and nerve function is particularly critical. It’s vital for muscle relaxation after contraction, preventing cramping, and for the transmission of nerve impulses. This ensures smooth communication between the brain and the rest of the body.
Potential Consequences of Magnesium Deficiency
Magnesium deficiency can manifest in a variety of ways, impacting various bodily systems. Mild deficiencies might exhibit symptoms like fatigue, muscle weakness, and irritability. More severe deficiencies can lead to more serious consequences, including seizures, heart problems, and bone loss. Early diagnosis and appropriate intervention are crucial in mitigating the negative impacts of magnesium deficiency.
Recommended Daily Intake of Magnesium
Adequate magnesium intake is essential for maintaining optimal health across different life stages. The recommended daily allowance varies based on age and gender. This table provides a general guideline for the recommended daily intake of magnesium:
| Age Group/Gender | Recommended Daily Intake (mg) |
|---|---|
| Men (19-30 years) | 400-420 |
| Women (19-30 years) | 320-360 |
| Men (31-50 years) | 420 |
| Women (31-50 years) | 320 |
| Men (51+ years) | 420 |
| Women (51+ years) | 320 |
| Pregnant Women | 350-400 |
| Lactating Women | 400 |
| Children (1-3 years) | 80-130 |
Note: These are general guidelines. Consult with a healthcare professional for personalized recommendations.
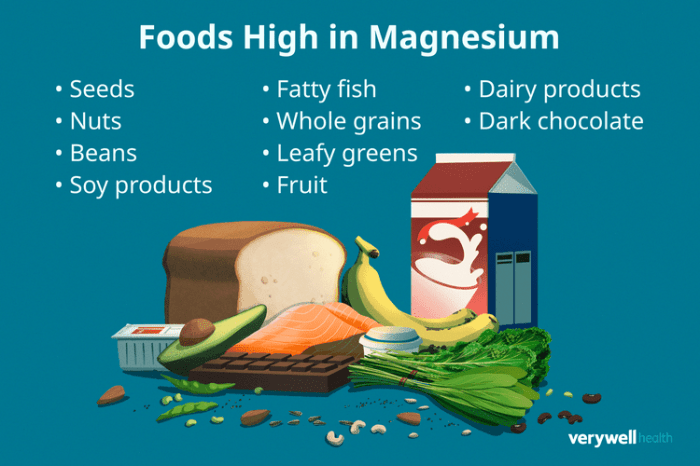
Foods High in Magnesium
Magnesium is a crucial mineral for numerous bodily functions, including muscle and nerve function, blood sugar regulation, and bone health. A diet rich in magnesium-rich foods can contribute significantly to overall well-being. Understanding which foods are excellent sources of this essential nutrient empowers you to make informed dietary choices.This section delves into a variety of foods packed with magnesium, offering insights into their nutritional value and preparation techniques to maximize magnesium retention.
We’ll also explore how preparation methods impact magnesium content and examine the magnesium levels in similar foods from different brands, providing you with valuable comparative data.
Magnesium-Rich Foods by Category
A diverse range of foods contribute to your daily magnesium intake. The following list highlights excellent sources, categorized for easier reference.
- Vegetables: Leafy greens like spinach, kale, and collard greens are excellent sources of magnesium. Other vegetables like broccoli, sweet potatoes, and asparagus also contain significant amounts. These nutrient-dense vegetables provide essential vitamins and minerals alongside magnesium.
- Fruits: Fruits like bananas, avocados, and dried figs are surprisingly good sources of magnesium. The unique combination of vitamins, minerals, and dietary fiber in these fruits further contributes to a balanced diet.
- Nuts and Seeds: Almonds, cashews, pumpkin seeds, and sunflower seeds are well-known for their magnesium content. These nutrient-dense snacks provide healthy fats and protein alongside magnesium.
- Legumes: Beans, lentils, and chickpeas are excellent plant-based protein sources and also contribute substantial amounts of magnesium. Their fiber content also aids digestion and promotes overall health.
- Whole Grains: Whole grains like quinoa, brown rice, and oats contain magnesium. These foods are also good sources of complex carbohydrates and fiber, contributing to sustained energy levels.
- Dairy Products: Certain dairy products like yogurt and milk provide some magnesium, though the amounts may vary depending on the specific product.
- Dark Chocolate: Dark chocolate, particularly with a high cocoa content, is a surprising source of magnesium. Its rich flavor profile and potential health benefits make it a delicious addition to a balanced diet.
Comparison of Magnesium Content in Food Groups
The table below illustrates the approximate magnesium content of various food groups. These values can fluctuate based on factors like growing conditions and preparation methods.
| Food Group | Approximate Magnesium Content (mg per 100g) |
|---|---|
| Leafy Greens | 50-150 |
| Fruits | 10-50 |
| Nuts and Seeds | 100-300 |
| Legumes | 30-80 |
| Whole Grains | 20-50 |
| Dairy Products | 10-30 |
Preserving Magnesium in Food Preparation
Proper preparation methods can help retain magnesium in foods. Avoid overcooking vegetables, as this can lead to magnesium loss. Steaming, stir-frying, or microwaving are gentler methods that can help maintain higher magnesium levels. Also, consider soaking or sprouting legumes before cooking to increase magnesium bioavailability.
Eating foods high in magnesium is crucial for overall health, and it plays a vital role in maintaining a healthy red blood cell rbc count. A balanced diet rich in magnesium-rich foods like spinach, almonds, and dark chocolate can significantly impact your body’s ability to produce healthy red blood cells. This, in turn, can positively influence various bodily functions.
For more detailed information on red blood cell rbc count, check out this informative article: red blood cell rbc count. Ultimately, incorporating these foods into your diet is a great way to support your body’s natural processes and overall well-being.
Comparison of Magnesium Content in Similar Foods from Different Brands
Comparing magnesium content across different brands of similar foods reveals variations. These differences can stem from factors like growing conditions, processing methods, and brand-specific nutritional fortification strategies. For instance, comparing different brands of almonds can show variations in magnesium content. Careful examination of nutritional labels is crucial to understand the magnesium content in your food choices.
| Food Item | Brand A | Brand B | Brand C |
|---|---|---|---|
| Almonds (100g) | 250mg | 270mg | 220mg |
| Spinach (100g) | 100mg | 90mg | 120mg |
| Brown Rice (100g) | 30mg | 35mg | 25mg |
Benefits of Magnesium-Rich Foods
Magnesium, a vital mineral, plays a crucial role in numerous bodily functions. Consuming foods rich in magnesium offers a multitude of health benefits, supporting everything from bone health to blood pressure regulation. Incorporating these foods into your diet can contribute to an overall improved sense of well-being and potentially reduce the risk of chronic diseases.Magnesium’s diverse actions within the body are remarkable.
It acts as a cofactor in hundreds of enzymatic reactions, impacting muscle function, nerve transmission, and blood sugar control. This wide-ranging influence underscores the importance of maintaining adequate magnesium intake through a balanced diet.
Blood Pressure Regulation
Magnesium plays a significant role in regulating blood pressure by promoting vasodilation, the widening of blood vessels. This relaxation of blood vessels reduces the resistance to blood flow, helping to lower blood pressure. Studies have shown a correlation between low magnesium intake and an increased risk of hypertension. Adequate magnesium intake can contribute to maintaining healthy blood pressure levels.
Bone Health
Magnesium is essential for bone health, directly influencing bone density and strength. It facilitates the absorption of calcium, a critical mineral for bone formation and maintenance. Sufficient magnesium intake, alongside calcium, is crucial for preventing osteoporosis and promoting healthy bones throughout life.
Overall Well-being
Magnesium’s role in muscle function and nerve transmission directly impacts overall well-being. Adequate magnesium levels can contribute to better sleep quality, reduced muscle cramps, and improved energy levels. These positive effects on daily functioning can significantly enhance the quality of life.
Magnesium-rich foods are fantastic for overall health, but did you know that regular sauna use can also significantly impact your magnesium levels? Effects of regular sauna use often lead to magnesium loss through sweat, so it’s crucial to replenish these levels through a balanced diet including foods like spinach, almonds, and dark chocolate. Prioritizing these foods helps maintain optimal magnesium levels for a healthy body.
Impact on Chronic Disease Risk Reduction
Maintaining adequate magnesium levels is linked to a reduced risk of developing chronic diseases. This is partly due to magnesium’s role in blood pressure regulation and its antioxidant properties, which can help protect cells from damage. Incorporating magnesium-rich foods into your diet can be a preventative measure against various chronic illnesses.
Magnesium and Specific Health Conditions
| Health Condition | Recommended Magnesium-Rich Foods |
|---|---|
| Premenstrual Syndrome (PMS) | Dark leafy greens, nuts, seeds, legumes, whole grains |
| Muscle Cramps | Spinach, almonds, cashews, pumpkin seeds |
| Osteoporosis | Leafy greens, legumes, seeds, almonds |
| Type 2 Diabetes | Spinach, broccoli, black beans, whole grains |
| High Blood Pressure | Dark leafy greens, avocados, bananas, nuts |
This table highlights some conditions where magnesium plays a key role and provides suggestions for magnesium-rich foods that may be beneficial. It’s important to remember that dietary changes should be discussed with a healthcare professional.
Dietary Considerations and Precautions
While magnesium is a vital nutrient, excessive intake can sometimes lead to unwanted side effects. Understanding how dietary choices and potential interactions with medications impact magnesium absorption is crucial for maintaining optimal health. This section explores potential downsides of overconsumption, factors influencing absorption, and possible medication interactions.Careful consideration of dietary factors and potential interactions with medications is essential for safe and effective magnesium supplementation.
By understanding these interactions, individuals can make informed choices to maximize the benefits of magnesium while minimizing risks.
Potential Side Effects of Excessive Magnesium Intake
Excessive magnesium intake, whether through supplements or a diet high in magnesium-rich foods, can cause a range of unpleasant side effects. These typically manifest as gastrointestinal issues, including diarrhea, nausea, and abdominal cramps. In severe cases, excessive magnesium can interfere with the absorption of other essential nutrients and potentially lead to cardiac arrhythmias or even kidney problems. Symptoms vary depending on the individual and the amount of magnesium consumed.
It’s important to note that individual tolerances vary significantly, and what one person can handle without issue another may not.
Factors Affecting Magnesium Absorption
Several dietary factors can influence how effectively the body absorbs magnesium. High fiber intake, for example, can bind with magnesium in the gut, reducing its absorption. Similarly, excessive consumption of certain foods can also hinder magnesium absorption. Calcium, in particular, competes with magnesium for absorption, and excessive calcium intake can lead to reduced magnesium levels. Other dietary factors, like high intakes of phytates (found in whole grains and legumes) and oxalates (present in spinach and rhubarb), can also limit magnesium absorption.
Foods That May Interfere with Magnesium Absorption
Certain foods contain compounds that can hinder the absorption of magnesium. High-fiber foods, like whole grains and beans, can bind with magnesium, reducing its bioavailability. Additionally, foods high in oxalates, such as spinach and rhubarb, and those high in phytates, like legumes and whole grains, can also impede magnesium absorption. These interactions are important to consider, especially for individuals who may already be deficient in magnesium.
Careful consideration of these foods alongside magnesium-rich foods is recommended for optimal intake.
Interactions Between Magnesium and Other Medications
Magnesium can interact with certain medications, potentially affecting their effectiveness or leading to adverse side effects. For instance, some medications used to treat heart conditions can interact with magnesium, potentially affecting heart rate or rhythm. Additionally, individuals taking diuretics may experience a loss of magnesium through urination, potentially requiring supplementation to maintain optimal levels. Individuals taking certain antibiotics may also experience interactions with magnesium, affecting the absorption of both.
Table of Potential Interactions
| Nutrient/Medication | Potential Interaction with Magnesium | Explanation |
|---|---|---|
| High Fiber Foods | Reduced Magnesium Absorption | Fiber can bind to magnesium, reducing its bioavailability. |
| High Calcium Foods | Reduced Magnesium Absorption | Calcium competes with magnesium for absorption. |
| High Oxalate Foods | Reduced Magnesium Absorption | Oxalates bind to magnesium, decreasing absorption. |
| High Phytate Foods | Reduced Magnesium Absorption | Phytates bind to magnesium, reducing its absorption. |
| Diuretics | Increased Magnesium Loss | Diuretics can increase magnesium excretion. |
| Certain Antibiotics | Potential Absorption Interference | Some antibiotics may affect magnesium absorption. |
| Certain Heart Medications | Potential Interactions | Certain heart medications may interact with magnesium levels. |
Practical Dietary Strategies: Foods High In Magnesium
Boosting your magnesium intake doesn’t have to feel like a chore. With a few smart strategies and delicious recipes, you can easily incorporate magnesium-rich foods into your daily meals, making it a sustainable part of your healthy lifestyle. By understanding how to prepare and store these foods, you can ensure you’re getting the full nutritional benefits.Integrating magnesium-rich foods into your diet effectively is crucial for optimal health and well-being.
It’s not just about eating more of these foods; it’s about understanding how to choose the right options, prepare them properly, and incorporate them seamlessly into your existing meal plan. This section delves into practical strategies for making magnesium-rich foods a regular part of your daily life.
Sample Meal Plan
This sample meal plan provides a framework for incorporating magnesium-rich foods into your daily diet. Adjust portion sizes based on your individual needs and preferences.
- Breakfast (e.g., Overnight Oats): Rolled oats, chia seeds, unsweetened almond milk, a handful of almonds, and a sprinkle of shredded coconut. This provides a good mix of complex carbohydrates, healthy fats, and magnesium.
- Lunch (e.g., Quinoa Salad): Cooked quinoa, chopped cucumber, tomatoes, bell peppers, chickpeas, and a lemon-herb vinaigrette. Quinoa is a complete protein source and a great source of magnesium.
- Dinner (e.g., Roasted Vegetables with Chickpeas): Roasted broccoli, carrots, sweet potatoes, and chickpeas seasoned with herbs and spices. This provides a variety of vegetables and legumes, all rich in magnesium.
- Snacks (e.g., Greek Yogurt with Berries): Greek yogurt with a mix of berries and a sprinkle of pumpkin seeds. Greek yogurt is a good source of protein and magnesium, while berries offer antioxidants.
Recipes Highlighting Magnesium
These recipes showcase delicious ways to use magnesium-rich ingredients.
- Spinach and Chickpea Curry: A hearty and flavorful curry with spinach and chickpeas, cooked in coconut milk and seasoned with turmeric, ginger, and garlic. Spinach is a fantastic source of magnesium, while chickpeas are also rich in it. This recipe can be easily adapted to suit your dietary preferences.
- Black Bean Burgers: Make your own black bean burgers using black beans, oats, and spices. Black beans are an excellent source of magnesium and fiber. These burgers can be served on whole-wheat buns with your favorite toppings.
Incorporating Magnesium-Rich Foods
Integrating magnesium-rich foods into your daily meals is easier than you might think.
- Breakfast Cereals: Choose cereals fortified with magnesium.
- Snacks: Reach for nuts, seeds, dried fruit, or yogurt.
- Side Dishes: Include leafy greens, legumes, and whole grains in your meals.
Storing and Preparing Magnesium-Rich Foods
Proper storage and preparation methods can help maintain the nutritional value of magnesium-rich foods.
- Leafy Greens: Store in the refrigerator and use within a few days. Avoid prolonged exposure to air.
- Legumes: Store dried legumes in a cool, dry place. Soak them properly before cooking to optimize nutrient absorption.
- Nuts and Seeds: Store in airtight containers in a cool, dark place. Avoid exposing them to heat or moisture.
Meal Type Incorporation Table
This table illustrates how to incorporate magnesium-rich foods into different meal types.
| Meal Type | Magnesium-Rich Food | Preparation/Incorporation Tip |
|---|---|---|
| Breakfast | Oatmeal, Spinach, Almonds | Add spinach to oatmeal, sprinkle almonds on top. |
| Lunch | Quinoa, Chickpeas, Leafy Greens | Make a salad with quinoa, chickpeas, and leafy greens. |
| Dinner | Legumes, Dark Leafy Greens, Whole Grains | Use legumes as a main dish or side dish. Include dark leafy greens in a stir-fry or salad. |
| Snacks | Nuts, Seeds, Dried Fruit | Carry a small bag of almonds or sunflower seeds for a quick snack. |
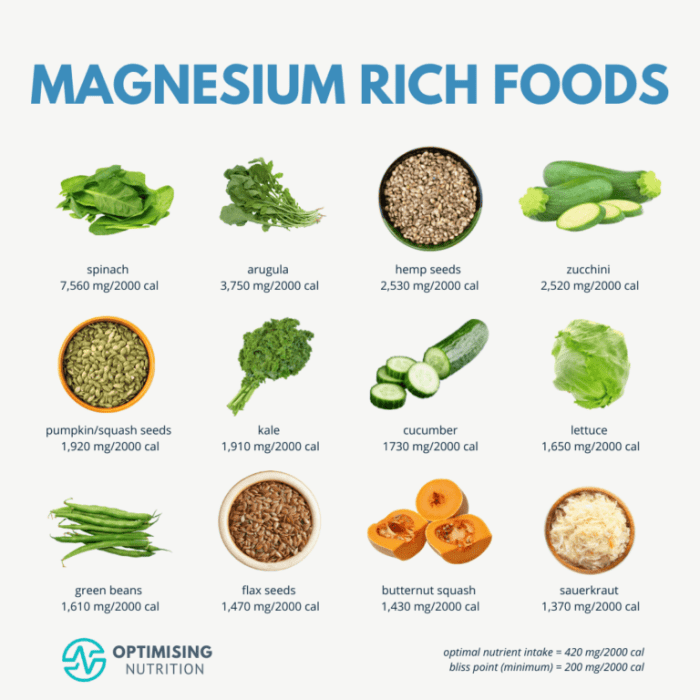
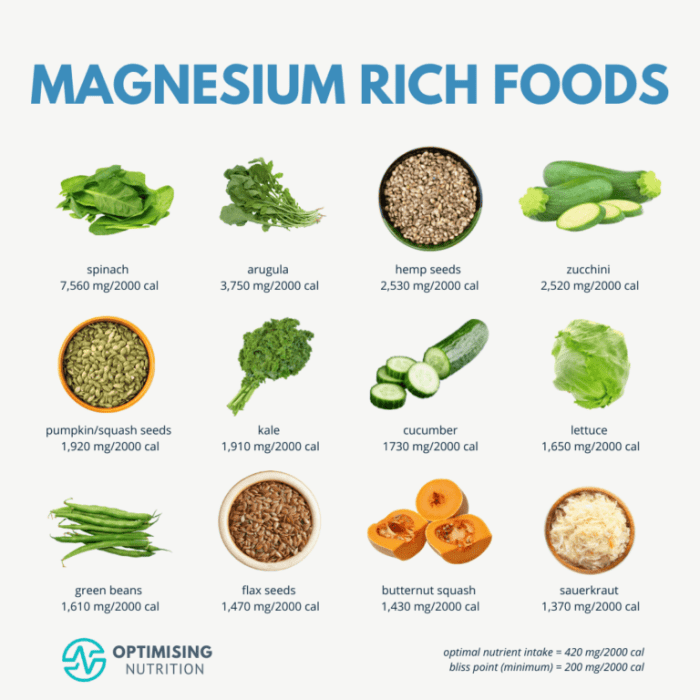
Visual Representation of Magnesium Content
Seeing is believing, especially when it comes to understanding essential nutrients like magnesium. Visual representations make complex nutritional information accessible and impactful. This section explores effective ways to showcase magnesium content, making it easier to grasp the importance of incorporating magnesium-rich foods into your diet.Visual aids are crucial for effectively communicating the value of magnesium. They allow for quick comprehension of nutritional data, empowering individuals to make informed dietary choices.
The following examples highlight various ways to present magnesium content in a digestible and engaging manner.
Top 10 Magnesium-Rich Foods Infographic
An infographic, ideally visually appealing and easily digestible, will effectively present the top 10 magnesium-rich foods. It should feature visually distinct icons or illustrations representing each food item, allowing for quick recognition. Color-coding, using a gradient from light to dark, can be used to visually represent increasing magnesium content. The infographic should also include concise labels for each food, its magnesium content per serving, and perhaps a small, easily digestible description of its nutritional benefits.
Magnesium Content Table
This table presents the magnesium content per serving for the top 10 magnesium-rich foods. It allows for a direct comparison of magnesium amounts across different foods. The table’s design should be clean and easy to read. Columns should include the food name, serving size, and the magnesium content in milligrams (mg).
| Food | Serving Size | Magnesium (mg) |
|---|---|---|
| Spinach | 1 cup cooked | 180 |
| Black Beans | 1 cup cooked | 160 |
| Almonds | 1/4 cup | 150 |
| Cashews | 1/4 cup | 120 |
| Avocado | 1 medium | 110 |
| Edamame | 1 cup | 100 |
| Pumpkin Seeds | 1/4 cup | 90 |
| Chia Seeds | 1 tbsp | 80 |
| Dark Chocolate (70% cacao or higher) | 1 oz | 70 |
| Plain Yogurt (Greek) | 1 cup | 60 |
Magnesium Content Bar Graph
A bar graph effectively compares the magnesium content of different food categories. For example, the graph could compare the average magnesium content per serving size for vegetables, legumes, nuts, seeds, and dairy products. Different colors can be used to represent each category, making visual comparisons quick and easy. The x-axis should represent the food category, and the y-axis should represent the magnesium content in milligrams.
This graph will provide a clear overview of which food groups are higher in magnesium.
Ideal Visual Representation for Nutritional Guide, Foods high in magnesium
For a nutritional guide, the ideal visual representation should prioritize clarity and accessibility. The presentation should be easily digestible and not overwhelming. Use a combination of infographics, tables, and graphs to present the information in various formats. The use of consistent color schemes and fonts across all visuals will create a cohesive and easily navigable guide. Clearly labeling units (mg, grams, cups) is crucial for accurate interpretation.
The information should be presented in a user-friendly way, enabling individuals to quickly and easily understand the magnesium content of different foods.
Closing Summary
In conclusion, incorporating foods high in magnesium into your diet is a powerful step towards overall well-being. By understanding the importance of magnesium, its diverse sources, and potential benefits, you can make informed choices to support your health. Remember, maintaining a balanced diet, rich in magnesium-rich foods, is key to achieving optimal health and vitality.