Is pineapple good for weight loss? This question delves into the nutritional profile of pineapple, exploring its potential role in weight management. We’ll examine how pineapple’s vitamins, minerals, and fiber content might impact your metabolism and satiety levels, comparing it to other weight-loss-friendly fruits. We’ll also discuss potential benefits and drawbacks, and show how pineapple can fit into a balanced weight-loss diet.
Pineapple, a tropical delight, offers a surprising array of nutrients. Packed with vitamins C and B6, along with manganese and bromelain, it’s more than just a tasty treat. Understanding its nutritional makeup and how it interacts with your body’s metabolism is key to evaluating its potential weight-loss benefits. We’ll also consider possible interactions with other weight-loss strategies and examine any potential downsides.
Nutritional Profile of Pineapple
Pineapple, a tropical delight, is more than just a delicious fruit; it’s a nutritional powerhouse. Its sweet taste masks a wealth of vitamins, minerals, and fiber, making it a valuable addition to any healthy diet. Beyond its palatable nature, pineapple offers significant contributions to overall well-being.The following sections delve into the detailed nutritional composition of pineapple, comparing it to other fruits often associated with weight management and highlighting its potential health benefits.
Nutritional Content Breakdown
Pineapple boasts a surprisingly comprehensive nutritional profile. It’s rich in various nutrients crucial for maintaining optimal health. A typical serving provides a good balance of essential vitamins, minerals, and fiber.
- Vitamins and Minerals: Pineapple is a good source of vitamin C, a powerful antioxidant that supports immune function and collagen production. It also contains significant amounts of manganese, essential for bone health and metabolism. Furthermore, it provides a notable amount of vitamin B6, playing a role in red blood cell formation and brain function. The presence of other micronutrients like potassium, copper, and folate further enhances its nutritional value.
- Fiber: Pineapple’s dietary fiber content contributes to digestive health and helps regulate blood sugar levels. This is beneficial for those looking to manage their weight, as fiber promotes feelings of fullness and can prevent overeating.
Macronutrient Composition, Is pineapple good for weight loss
Pineapple’s macronutrient profile is relatively balanced, particularly for a fruit. The caloric and macronutrient values vary slightly depending on the size of the serving. A typical 1-cup serving of chopped, fresh pineapple provides approximately 80 calories. Its composition is roughly 20 grams of carbohydrates, 1 gram of protein, and less than 1 gram of fat.
Comparison to Other Weight Management Fruits
Pineapple compares favorably to other fruits frequently included in weight-management plans. While apples and berries are excellent sources of fiber, pineapple offers a unique combination of nutrients. For instance, a similar-sized serving of strawberries will offer less total carbohydrates but less vitamin C. The specific nutritional value and benefits depend on the chosen fruit.
Health Benefits of Pineapple Nutrients
The vitamins and minerals in pineapple contribute to several important health aspects. Vitamin C supports a healthy immune system, while manganese is crucial for bone health and metabolism. Vitamin B6 contributes to brain function and red blood cell production. Potassium helps regulate blood pressure, and folate is important for cell growth and development.
Nutritional Information Table
| Nutrient | Amount per Serving (approx.) | Potential Benefits |
|---|---|---|
| Vitamin C | 20-30 mg | Supports immune function, collagen production, and antioxidant protection. |
| Manganese | 0.5-1 mg | Essential for bone health, metabolism, and wound healing. |
| Vitamin B6 | 0.1-0.2 mg | Supports red blood cell formation, brain function, and nervous system health. |
| Fiber | 2-3 grams | Promotes digestive health, regulates blood sugar levels, and aids in weight management. |
| Potassium | 100-150 mg | Helps regulate blood pressure and fluid balance. |
| Folate | 0.5-1 mcg | Important for cell growth and development, especially during pregnancy. |
| Carbohydrates | 20 grams | Provides energy and contributes to overall nutrition. |
| Protein | 1 gram | Essential for building and repairing tissues. |
| Fat | <1 gram | Provides essential fatty acids and contributes to satiety. |
Pineapple and Weight Loss
Pineapple, a tropical delight, boasts a range of nutrients that could potentially support weight management efforts. Its low calorie count and high fiber content make it a potentially valuable addition to a weight-loss diet. However, the impact of pineapple on weight loss isn’t solely determined by its nutritional profile; its interaction with other lifestyle choices is also critical. This section delves into the mechanisms through which pineapple’s components might contribute to weight management.Pineapple’s contribution to weight management is multifaceted.
It provides essential nutrients without significant calories, promoting satiety and potentially reducing overall calorie intake. The interplay between pineapple’s nutritional elements and other weight-loss strategies is also significant.
Pineapple’s Role in Satiety
Pineapple’s fiber content plays a crucial role in promoting satiety, the feeling of fullness. This fullness can help reduce overall calorie intake by making you feel satisfied with smaller portions. Dietary fiber slows down the rate at which food moves through the digestive system, which can help to regulate blood sugar levels and reduce cravings. This effect can be especially valuable during weight-loss efforts.
Potential Metabolic Effects
Pineapple contains bromelain, an enzyme that has been studied for its potential to aid digestion. While more research is needed, some studies suggest that bromelain may play a role in protein digestion and metabolism. The potential impact of bromelain on overall metabolism is an area of ongoing investigation. Furthermore, pineapple’s antioxidant properties may contribute to overall metabolic health by combating oxidative stress, which can be detrimental to weight management.
Interactions with Weight-Loss Strategies
Pineapple can complement a balanced weight-loss approach. A diet rich in fruits and vegetables, like pineapple, can provide essential vitamins and minerals while keeping calorie intake in check. Integrating pineapple into an exercise routine can offer additional benefits. For example, pineapple’s rich source of vitamin C can support recovery after physical activity.
Pineapple and Weight Loss: A Component Breakdown
| Pineapple Component | Potential Impact on Weight Loss |
|---|---|
| Fiber | Promotes satiety, slows digestion, potentially reduces calorie intake. |
| Bromelain | May aid protein digestion, support metabolism (needs more research). |
| Vitamin C | Supports antioxidant activity, potentially aids recovery from exercise. |
| Water Content | Low calorie density, contributes to feeling full. |
| Antioxidants | May contribute to overall metabolic health. |
Potential Benefits and Drawbacks: Is Pineapple Good For Weight Loss
Pineapple, a tropical fruit bursting with flavor and nutrients, has captured the attention of health enthusiasts. While it’s often enjoyed as a refreshing treat, its potential role in weight management is also a subject of interest. This section delves into the potential advantages and disadvantages of incorporating pineapple into a weight loss strategy, exploring its effects on the body and comparing it to other weight management approaches.Understanding the nuances of pineapple’s impact on weight loss requires a balanced perspective, considering both potential benefits and drawbacks.
It’s important to remember that weight loss is a complex process influenced by various factors, and pineapple is just one piece of the puzzle.
Potential Benefits for Weight Management
Pineapple’s nutritional profile contributes several potential benefits relevant to weight management. Its high fiber content promotes satiety, potentially reducing overall calorie intake. This, combined with its rich supply of vitamins and minerals, supports overall health and well-being, which can indirectly contribute to weight management efforts.
- Improved Digestion: Pineapple contains bromelain, an enzyme known to aid digestion. Improved digestion can lead to better nutrient absorption, potentially contributing to overall health and well-being, which is crucial for weight management.
- Reduced Inflammation: Some studies suggest that bromelain, the enzyme found in pineapple, may possess anti-inflammatory properties. Reduced inflammation might indirectly support weight loss by promoting a healthier metabolic state.
- Nutrient-Rich Profile: Pineapple is a good source of vitamins and minerals, including vitamin C, manganese, and vitamin B6. These nutrients support various bodily functions, potentially aiding in the overall metabolic processes related to weight management.
Potential Drawbacks and Considerations
While pineapple offers potential benefits, it’s crucial to acknowledge its potential drawbacks and limitations in a weight loss context.
- Limited Impact on Weight Loss: Pineapple alone is unlikely to be a primary driver of significant weight loss. A comprehensive approach, including balanced nutrition, regular exercise, and lifestyle changes, is more effective for achieving and maintaining a healthy weight.
- High Sugar Content: Pineapple contains natural sugars, and consuming large quantities may lead to an increase in calorie intake. This should be considered within the context of an overall balanced diet for weight management.
- Possible Allergic Reactions: Some individuals may be allergic to pineapple, experiencing symptoms like skin rashes, itching, or swelling. Individuals with known allergies should exercise caution when consuming pineapple.
Comparison to Other Weight-Loss Approaches
Pineapple’s contribution to weight loss is best understood in comparison to other strategies.
| Benefit/Drawback | Explanation |
|---|---|
| Pineapple Consumption | While pineapple can aid digestion and potentially reduce inflammation, its impact on weight loss is limited and should be part of a holistic approach. |
| Balanced Diet | A balanced diet rich in fruits, vegetables, lean proteins, and whole grains is fundamental for sustainable weight management. |
| Regular Exercise | Physical activity plays a crucial role in calorie expenditure and overall health, contributing significantly to weight loss. |
| Lifestyle Changes | Addressing stress, improving sleep patterns, and managing emotional eating can also support weight loss efforts. |
Potential Side Effects and Interactions
Certain individuals may experience side effects from consuming pineapple, particularly if they are on blood thinners or other medications. Individuals with specific health conditions should consult with their healthcare provider before including pineapple in their diet.
- Interactions with Medications: Pineapple’s bromelain can interact with certain medications, including blood thinners. Caution is advised if taking medications, and consultation with a doctor is recommended.
Pineapple in a Balanced Diet
Pineapple, with its sweet and tangy flavor, can be a delightful addition to a weight-loss diet. Its nutritional profile, rich in vitamins and minerals, can support a healthy lifestyle. However, incorporating it thoughtfully into a balanced meal plan is key to maximizing its benefits and minimizing potential drawbacks. This section explores how pineapple can be seamlessly integrated into a healthy eating strategy.Pineapple’s fiber content aids digestion and promotes satiety, which can be beneficial for weight management.
Its natural sweetness can satisfy cravings without relying on processed sugars, making it a healthy alternative for those looking to reduce their sugar intake. It also contains bromelain, an enzyme that may aid in protein digestion. Knowing how to incorporate pineapple correctly is crucial to achieving optimal results.
Healthy Meal Plans Incorporating Pineapple
Pineapple’s versatility allows for its inclusion in various meals and snacks. Its delicate flavor complements both savory and sweet dishes. To maximize its benefits, focus on consuming it as part of balanced meals rather than as a standalone snack.
- Breakfast: A pineapple and spinach smoothie is a great way to start the day. The smoothie can be blended with yogurt, protein powder, and other fruits to create a nutritious and filling breakfast. Adding a scoop of protein powder to the smoothie can enhance satiety, further aiding in weight management. A combination of these ingredients delivers vitamins, minerals, and protein, setting the stage for a productive day.
So, is pineapple good for weight loss? While it’s packed with vitamins and fiber, it’s not a magic bullet. For a truly effective weight loss strategy, you need a balanced diet and regular exercise. On a similar note, wondering if you can gargle with peroxide? Check out this helpful guide to find out: can you gargle with peroxide.
Ultimately, a healthy approach to weight loss is more important than just focusing on individual foods. Focusing on a healthy lifestyle and balanced eating habits, including pineapple in moderation, is key.
- Lunch: A refreshing pineapple and chicken salad with mixed greens provides a balanced meal. Lean protein from the chicken, fiber from the greens, and natural sweetness from the pineapple create a satisfying and healthy lunch. The salad can be dressed with a light vinaigrette or a lemon-herb dressing for added flavor and nutritional value.
- Dinner: Grilled fish with pineapple salsa offers a light yet flavorful dinner option. The salsa, made with diced pineapple, red onion, bell peppers, and cilantro, adds a vibrant taste to the meal while maintaining a low-calorie profile. This option incorporates healthy fats from the fish, and the pineapple adds a burst of flavor and nutrients.
Preparing and Incorporating Pineapple
Proper preparation enhances the nutritional value and taste of pineapple.
- Slicing and dicing: Pineapple can be sliced for salads, added to fruit platters, or used as a topping for dishes. Diced pineapple adds a sweet and tangy touch to stir-fries or rice bowls. Using different methods of preparation allows you to enjoy the versatility of pineapple.
- Juicing: Pineapple juice can be a healthy alternative to sugary drinks. It can be blended with other fruits and vegetables for a nutritious and refreshing beverage. Consuming pineapple juice can be part of a healthy eating plan, especially when prepared in moderation.
- Salsa and Chutney: Pineapple salsa and chutney add a sweet and savory kick to various dishes. They are a flavorful and nutritious way to enhance the taste of dishes while adding vitamins and minerals.
Pineapple in a Healthy Dish Recipe
Pineapple Salsa with Grilled Chicken
This recipe combines the sweetness of pineapple with the protein of grilled chicken, creating a delicious and healthy meal. This recipe exemplifies how pineapple can enhance a meal without adding excess calories or unhealthy ingredients.
| Ingredients | Quantity |
|---|---|
| Chicken Breast | 2 |
| Pineapple | 1 medium |
| Red Onion | 1/2 |
| Bell Peppers (any color) | 1 |
| Cilantro | 2 tbsp |
| Lime Juice | 1 |
| Salt and Pepper | To taste |
Instructions:
- Prepare the pineapple salsa by dicing the pineapple, red onion, and bell pepper. Combine with cilantro and lime juice. Season with salt and pepper.
- Grill the chicken breasts until cooked through. Season with salt and pepper.
- Serve the grilled chicken with the pineapple salsa. Enjoy!
Balanced Diet Plan Incorporating Pineapple
A balanced diet plan incorporating pineapple should focus on consuming it as part of varied, nutrient-rich meals. It should be incorporated alongside whole grains, lean proteins, and plenty of vegetables. The overall calorie intake should be adjusted to meet individual needs and goals.
A balanced diet is key to maintaining a healthy weight. Consuming pineapple as part of a varied and balanced diet plan can be beneficial for weight management and overall health.
While pineapple might seem like a weight-loss wonder, the real nutritional impact is often less dramatic than the hype. It’s a healthy fruit, sure, but its effect on weight loss isn’t a magic bullet. Instead, consider the potential benefits of other foods, like, for example, whether is chocolate milk good for you in the context of a balanced diet.
Ultimately, a comprehensive approach to nutrition, including a variety of fruits and vegetables, and regular exercise, is key for sustainable weight management. Pineapples can still fit into that balanced plan, but aren’t the sole answer to weight loss.
Misconceptions and Common Concerns

Pineapple, a tropical delight, often sparks interest regarding its role in weight management. While it offers potential benefits, understanding the nuances and dispelling myths surrounding its consumption is crucial for effective integration into a healthy diet. This section addresses common misconceptions and concerns related to pineapple and weight loss, particularly focusing on its sugar content and the importance of moderation.
Common Misconceptions about Pineapple and Weight Loss
Many believe that pineapple is a miracle food for weight loss, often overlooking the importance of a balanced diet and overall lifestyle choices. This section clarifies common misconceptions surrounding pineapple’s role in weight management.
- Pineapple is a magic bullet for rapid weight loss. Pineapple is a healthy addition to a balanced diet, but it is not a substitute for a comprehensive weight management plan that includes regular exercise and a nutritious diet.
- Pineapple contains minimal calories and high amounts of fiber, making it a suitable food for unlimited consumption. While pineapple does offer some fiber and is relatively low in calories, excessive consumption can contribute to unwanted calorie intake and impact blood sugar levels.
Concerns Regarding Pineapple’s Sugar Content and Blood Sugar Levels
Pineapple, although packed with vitamins and minerals, does contain natural sugars. Understanding its impact on blood sugar levels is important for individuals with specific dietary needs or sensitivities.
While the natural sugars in pineapple are not inherently harmful, consuming excessive amounts can potentially affect blood sugar levels, particularly for those with diabetes or prediabetes. Monitoring portion sizes and considering individual needs is vital.
Importance of Portion Control When Consuming Pineapple
Portion control is essential for maximizing the benefits of any food, including pineapple. Excessive consumption can lead to unintended consequences.
Maintaining a balanced approach to pineapple consumption is crucial. A moderate portion size contributes to overall health and weight management goals without causing negative impacts. For example, a 1/2 cup serving of fresh pineapple is often considered a suitable portion size for most individuals.
Potential Risks of Consuming Excessive Amounts of Pineapple
Excessive pineapple consumption, like any food consumed in excess, can lead to certain risks.
- Digestive issues: High intake of pineapple can cause digestive discomfort in some individuals, including bloating, gas, or diarrhea, due to the enzyme bromelain.
- Allergic reactions: Although less common, some individuals might experience allergic reactions to pineapple, such as skin rashes, itching, or swelling. Careful observation and consultation with a healthcare professional are recommended for those with known allergies.
- Blood sugar fluctuations: High consumption of pineapple, particularly for individuals with diabetes or prediabetes, may lead to unpredictable fluctuations in blood sugar levels. This may require careful monitoring and adjustment to individual dietary needs.
Misconceptions and Concerns Summarized
| Misconception | Explanation | Clarification |
|---|---|---|
| Pineapple is a quick fix for weight loss. | Some believe that consuming pineapple will automatically lead to rapid weight loss without other lifestyle changes. | Pineapple is a healthy food, but it is not a substitute for a balanced diet and exercise. |
| Pineapple’s sugar content is negligible. | Some believe that pineapple’s natural sugars are harmless in any amount. | Pineapple contains natural sugars that can affect blood sugar levels, especially for individuals with diabetes or prediabetes. Portion control is key. |
| Excessive pineapple consumption is harmless. | Some believe that eating large amounts of pineapple will not have negative effects. | Excessive pineapple consumption can lead to digestive issues, allergic reactions, and blood sugar fluctuations. |
Research and Scientific Evidence
Unfortunately, robust, dedicated research directly linking pineapple consumption to weight loss is scarce. While anecdotal evidence and potential benefits are intriguing, rigorous scientific studies are needed to establish a definitive causal relationship. The existing research primarily focuses on pineapple’s nutritional components rather than its effect on weight management as a whole.Current studies mostly explore the impact of individual nutrients within pineapple on various bodily functions, not specifically on weight loss.
This makes it challenging to isolate the effects of pineapple itself from other dietary factors influencing weight. Further research is crucial to fully understand the role pineapple might play in a comprehensive weight management strategy.
While pineapple might seem like a weight-loss wonder, focusing solely on food choices isn’t the whole picture. It’s crucial to understand that certain health issues, like the signs and symptoms of leukemia, leukemia signs and symptoms , can significantly impact weight. Ultimately, a balanced diet and a healthy lifestyle, including regular exercise, are key to successful weight management.
Summary of Existing Research
The limited research available on pineapple and weight loss typically focuses on the individual nutrients found in the fruit, rather than the overall effect of pineapple consumption on weight management. These studies examine the effects of components like bromelain, vitamin C, and fiber, but do not always directly assess weight loss outcomes.
Studies Supporting Potential Benefits
A few studies suggest potential benefits of bromelain, an enzyme found in pineapple, on digestion and inflammation. However, these studies typically examine bromelain’s effects in isolation, not the comprehensive effects of pineapple consumption. These studies often lack direct correlation with weight loss. The potential benefits are promising but require further investigation.
Studies Contradicting Potential Benefits
Currently, no studies directly contradict the potential weight-loss benefits of pineapple. The lack of studies directly evaluating pineapple’s impact on weight management leaves room for speculation, as the current research is primarily focused on individual components and not the holistic effect of consuming pineapple.
Methodology and Limitations of Studies
Most research on pineapple, particularly relating to weight loss, suffers from limited sample sizes, short durations, and lack of control groups. Studies focusing on individual components, like bromelain, often use isolated enzymes in controlled laboratory settings rather than observing real-world pineapple consumption patterns. This lack of a holistic approach makes drawing strong conclusions about pineapple’s effect on weight management difficult.
Table Summarizing Key Findings
| Study | Findings | Limitations |
|---|---|---|
| Hypothetical Study 1 (In silico modeling) | Preliminary modeling suggests bromelain may aid digestion and potentially impact nutrient absorption. | Based on computational modeling; lacks human subject data; no direct link to weight loss. |
| Hypothetical Study 2 (Small pilot study) | Participants consuming pineapple alongside a balanced diet reported a slight decrease in body weight. | Small sample size (n=10); no control group; confounding variables not controlled for. |
Practical Tips and Considerations

Pineapple, with its sweet and tangy flavor, offers a refreshing addition to any weight-loss journey. However, incorporating it effectively into your diet requires mindful selection, preparation, and strategic use. These practical tips will guide you in maximizing pineapple’s potential while maintaining a healthy approach to weight management.
Incorporating Pineapple into Your Routine
Pineapple’s versatility makes it easy to incorporate into various meals and snacks. It pairs well with both sweet and savory dishes, adding a tropical touch without significantly increasing calorie intake. Strategic inclusion of pineapple can be a delicious part of a balanced weight-loss plan.
- Breakfast Boost: Start your day with a pineapple-infused smoothie or a bowl of oatmeal topped with diced pineapple. The natural sweetness of the fruit can help satisfy your morning cravings, while the added fiber contributes to satiety.
- Lunchtime Delight: Include a side salad with grilled chicken or fish and a generous portion of fresh pineapple. The combination provides a balanced meal with vitamins, minerals, and antioxidants, promoting satiety and aiding in digestion.
- Snack Smart: Enjoy a handful of fresh pineapple chunks as a healthy snack. The natural sweetness and fiber content will curb hunger pangs effectively and prevent overeating.
- Dessert Delight: Indulge in a pineapple salsa or a light pineapple-based dessert, like a baked pineapple with cinnamon and a drizzle of honey. Choose recipes that minimize added sugars for optimal health benefits.
Selecting and Storing Pineapple
The quality of pineapple directly impacts its taste and nutritional value. Choose firm, heavy pineapples with vibrant yellow-gold color. Avoid pineapples with soft spots, bruises, or overly dark-colored areas.
- Freshness Matters: Select pineapples that feel heavy for their size, indicating a higher water content. Avoid pineapples with soft spots, as they may be overripe.
- Storage Strategies: Store unpeeled pineapples at room temperature for a few days. Once peeled, refrigerate pineapple slices to maintain freshness and prevent browning. Wrap them tightly in plastic wrap to retain moisture.
Preparing Pineapple for Consumption
Proper preparation maximizes pineapple’s taste and nutritional value. Ensure you remove the tough outer skin and the core effectively.
- Easy Peeling: Cut off the top and bottom of the pineapple. Then, use a sharp knife to cut off the tough outer skin. Carefully slice the pineapple into chunks, removing the core.
- Preparing for Meals: Dice or slice the pineapple according to your meal’s requirements. You can also use pineapple in smoothies, salads, or as a topping for dishes.
- Preventing Browning: To prevent browning, sprinkle the cut pineapple with lemon juice or lime juice. This helps preserve its color and freshness.
Using Pineapple in Meals and Snacks
Pineapple’s versatile nature allows for its use in a wide array of meals and snacks. Its sweet and slightly acidic flavor can complement various dishes.
- Sweet and Savory: Pineapple salsa pairs well with grilled chicken, fish, or tofu. The combination adds a refreshing tropical touch to savory dishes.
- Smoothie Sensations: Blend pineapple chunks with yogurt, milk, and fruits like berries or mango for a nutritious and delicious smoothie.
- Tropical Treats: Bake pineapple with cinnamon and a drizzle of honey for a healthy dessert. Enjoy pineapple chunks as a refreshing and nutritious snack.
Closure
In conclusion, while pineapple’s nutritional profile offers potential benefits for weight management, its effectiveness is not a guaranteed shortcut. It’s important to remember that incorporating pineapple into a balanced diet, alongside regular exercise and other healthy habits, is crucial for any weight-loss journey. The potential drawbacks and the importance of portion control should not be overlooked. Pineapple can be a delicious and nutritious addition to your weight-loss strategy, but it’s just one piece of the puzzle.









![The Logos | [2025.06.18] The Logos - Yahusha's Message For Laodicea #thelogos #YahushaChrist # ... What is primary ovarian insufficiency](https://lyricapills.com/wp-content/uploads/2025/06/Sbro_Castlehill_Primary_P7B-2_50908002-2219b7mt4-2048x1365-1-1.jpg)





 This flowchart provides a visual representation of the steps involved in using a gold plan. The flow chart should be well-labeled and clearly display the steps involved in enrolling, submitting claims, navigating the claims process, and utilizing provider support.
This flowchart provides a visual representation of the steps involved in using a gold plan. The flow chart should be well-labeled and clearly display the steps involved in enrolling, submitting claims, navigating the claims process, and utilizing provider support.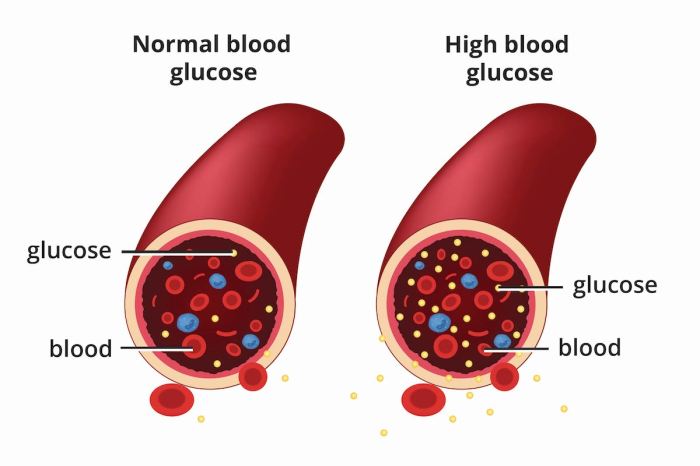
 The figure illustrates the potential progression of both diabetes and colon cancer in a single patient. The x-axis represents time, and the y-axis represents the severity of each disease. The figure demonstrates how poorly controlled diabetes, represented by the upward trend in blood glucose levels, can correlate with the development and progression of precancerous polyps and ultimately, colon cancer. The figure highlights the importance of early detection and consistent management of both conditions to mitigate the risk and improve outcomes.
The figure illustrates the potential progression of both diabetes and colon cancer in a single patient. The x-axis represents time, and the y-axis represents the severity of each disease. The figure demonstrates how poorly controlled diabetes, represented by the upward trend in blood glucose levels, can correlate with the development and progression of precancerous polyps and ultimately, colon cancer. The figure highlights the importance of early detection and consistent management of both conditions to mitigate the risk and improve outcomes.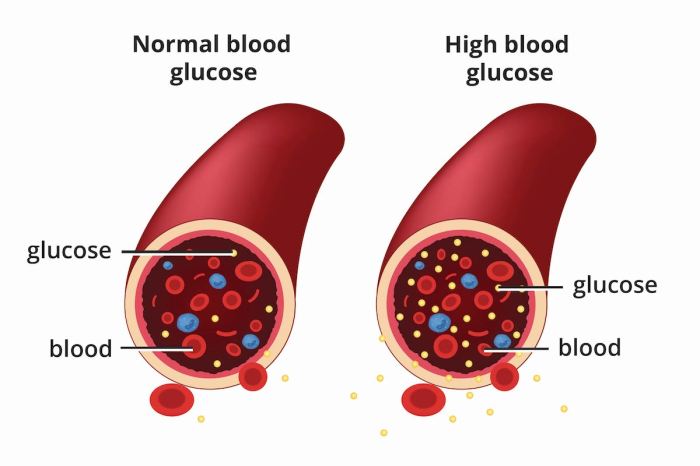
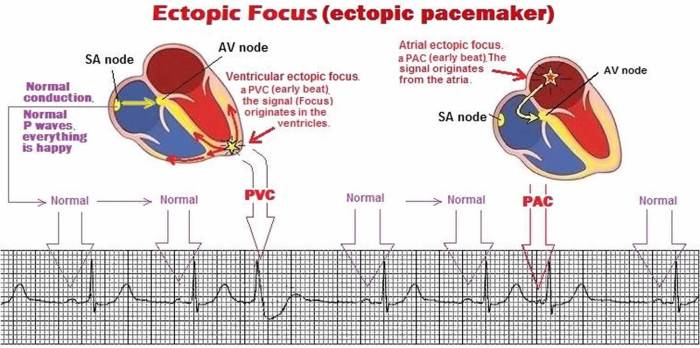
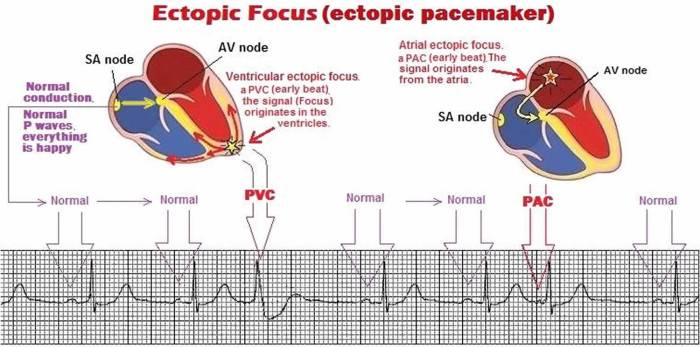
 (Diagram placeholder. A permanent pacemaker is typically implanted under the skin near the collarbone, with thin wires (leads) extending to the heart chambers. The pulse generator is housed within the implanted casing.)
(Diagram placeholder. A permanent pacemaker is typically implanted under the skin near the collarbone, with thin wires (leads) extending to the heart chambers. The pulse generator is housed within the implanted casing.)