Radial scars a benign breast abnormality – Radial scars, a benign breast abnormality, often present as a somewhat mysterious finding on mammograms or ultrasounds. They can mimic certain malignant breast conditions, leading to anxiety and uncertainty for patients. Understanding the characteristics, diagnostic processes, and management strategies surrounding radial scars is crucial for both healthcare professionals and those affected. This exploration delves into the intricacies of these breast lesions, providing a comprehensive overview.
Radial scars are benign breast lesions that typically appear as a star-shaped or spoke-like structure within the breast tissue. They are characterized by the presence of radiating fibrous tissue, which may or may not be accompanied by some glandular tissue. This article will explore the various aspects of radial scars, from their definition and presentation to diagnostic approaches, management strategies, and patient impact.
Introduction to Radial Scars: Radial Scars A Benign Breast Abnormality
Radial scars are benign (non-cancerous) breast abnormalities characterized by a star-shaped pattern of fibrous tissue growth radiating outward from a central point. They are a common finding in mammograms, often detected incidentally. These scars are typically asymptomatic, meaning they don’t cause any noticeable pain or discomfort. However, they can sometimes be associated with a slightly increased risk of breast cancer, though this risk is generally considered low.The typical presentation of a radial scar involves a collection of dense fibrous tissue strands within the breast.
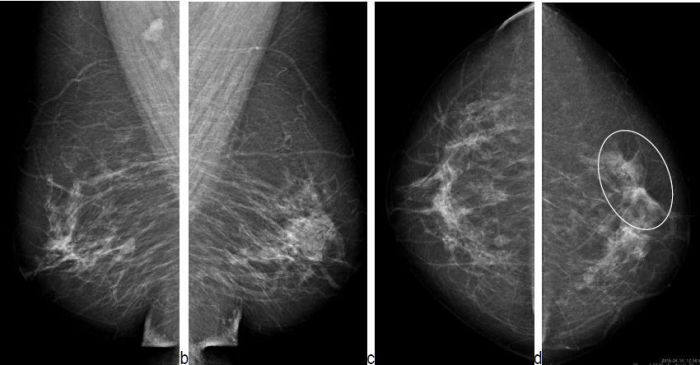
These strands appear as a starburst or spoke-like pattern on mammograms, and can also be visible on ultrasound. The characteristics of a radial scar can vary, with some being relatively simple and others more complex. The presence of associated microcalcifications, or small mineral deposits, can also be observed in some cases.Radial scars can be located anywhere within the breast tissue.
They are not limited to specific areas and can appear in the upper, lower, inner, or outer portions of the breast. Their distribution is fairly random and not tied to any particular breast quadrant. Mammographic assessment is essential for precise localization.
Radial scars, a benign breast abnormality, can sometimes be concerning. Understanding the nature of these scars is key, and it’s important to remember they’re often nothing to worry about. However, if you’re experiencing emotional distress related to this finding, exploring options like interpersonal therapy might be beneficial. What is interpersonal therapy can help address emotional challenges surrounding a medical diagnosis.
Ultimately, a thorough understanding of radial scars, coupled with support systems like the ones interpersonal therapy can provide, helps patients manage the experience and maintain emotional well-being.
Types of Radial Scars
Understanding the different types of radial scars helps in appropriate diagnostic and management strategies. The classification of radial scars can be based on their complexity and the extent of the involved tissue.
| Type | Description |
|---|---|
| Simple Radial Scar | Characterized by a well-defined, relatively straightforward pattern of radiating fibrous tissue. The fibrous strands are generally organized and exhibit a clear, discernible central point. Simple scars often present with a limited area of involvement. |
| Complex Radial Scar | Involves a more extensive and less organized pattern of fibrous tissue. The radiating strands might be less distinct or overlap, creating a more diffuse and intricate pattern. The involved area is typically larger than in simple radial scars, and may show a more significant degree of architectural distortion. |
Differentiating Radial Scars from Malignancy
Radial scars, while benign, can sometimes mimic malignant breast lesions. Accurate differentiation is crucial for appropriate patient management. This involves careful consideration of clinical history, physical examination findings, and imaging characteristics. This section will delve into the key distinctions between radial scars and breast cancers, highlighting overlapping features with other benign conditions.Differentiating radial scars from malignant breast lesions relies on a combination of clinical assessment and imaging analysis.
A thorough understanding of the characteristics unique to each entity is paramount for avoiding unnecessary biopsies and ensuring accurate diagnosis. The subtle distinctions between benign and malignant conditions can be challenging to identify, but careful attention to detail can significantly improve diagnostic accuracy.
Clinical Features Distinguishing Radial Scars
Clinical examination plays a vital role in the initial assessment. Radial scars typically present as a palpable, well-circumscribed mass, often firm or hard in consistency. They may be associated with nipple retraction or skin dimpling in some cases. Conversely, malignant breast lesions may present with similar palpable findings, but may also exhibit skin ulceration, nipple discharge, or inflammatory changes, which are less common in radial scars.
It’s important to note that these are not exclusive characteristics and overlap can occur.
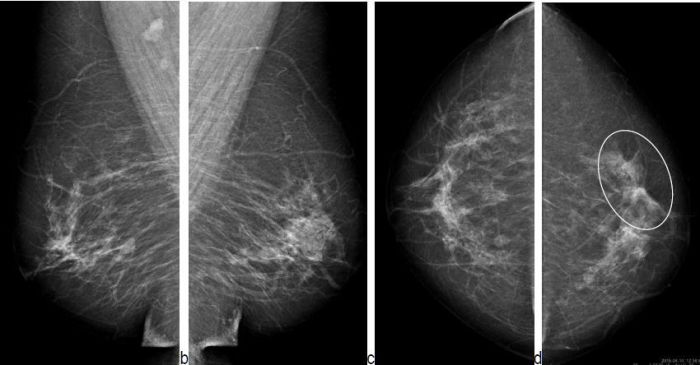
Imaging Findings: Mammography, Ultrasound, and MRI
Mammography, ultrasound, and MRI provide valuable imaging data. Mammographically, radial scars appear as a stellate or spoke-like configuration of densities, often with a central, dense area. Ultrasound may reveal a well-defined, hypoechoic or isoechoic mass with a characteristic pattern that often helps differentiate from malignant lesions. MRI findings may also help differentiate radial scars from malignancy. In some cases, radial scars demonstrate a non-enhancing or mildly enhancing appearance on MRI, while malignant lesions typically exhibit a more intense and heterogeneous enhancement pattern.
These are general trends and exceptions exist.
Overlapping Characteristics with Other Benign Conditions
Some benign breast conditions may share overlapping characteristics with radial scars. Fibroadenomas, for example, can present as palpable masses, and some may exhibit similar imaging features. Careful correlation between clinical findings and imaging characteristics is essential in these cases. The presence of specific features, like a distinct stellate pattern on mammography, may suggest a radial scar over other benign conditions.
Comparison of Mammographic Appearances
| Feature | Radial Scar | Breast Cancer |
|---|---|---|
| Shape | Stellate (spoke-like), often with a central dense area | Irregular, spiculated, or circumscribed |
| Margins | Well-defined | Often irregular or poorly defined |
| Density | May vary from dense to less dense | May vary, but often more dense than surrounding tissue |
| Calcifications | May or may not have calcifications, if present, typically coarse | Calcifications may be present, but often have a different appearance, often fine or microcalcifications |
| Associated findings | Nipple retraction or skin dimpling (possible) | Nipple discharge, skin ulceration, inflammatory changes (possible) |
Diagnostic Procedures and Workup
Radial scars, while benign, require careful evaluation to rule out malignancy and ensure appropriate management. A multi-faceted approach combining imaging, clinical history, and physical examination is crucial for accurate diagnosis and subsequent treatment planning. This process involves a series of steps that are designed to differentiate radial scars from potentially more serious conditions.
Imaging Modalities
Imaging plays a vital role in the diagnostic workup of radial scars. Mammography, ultrasound, and MRI are the primary imaging modalities used. Mammography, the standard initial screening tool, often reveals a dense, stellate (star-shaped) area of tissue. Ultrasound can provide further details about the lesion’s characteristics, including its size, shape, and internal structure. MRI, particularly MRI with contrast, is often considered the most informative imaging modality.
Radial scars, a benign breast abnormality, can sometimes be concerning. Understanding the potential impact of supplements like magnesium citrate is important, especially when considering how long it stays in your system. For example, knowing how long does magnesium citrate stay in your system can help with dosage planning and potentially alleviate some anxiety related to these breast conditions.
Ultimately, though, a healthcare professional should always be consulted for diagnosis and treatment related to radial scars.
It can depict the extent of the radial scar, its relationship to surrounding tissues, and provide valuable information about the surrounding breast tissue. The combination of these imaging techniques allows for a comprehensive assessment of the lesion and surrounding breast structures.
Clinical History and Physical Examination
Thorough clinical history taking and physical examination are integral components of the diagnostic process. A detailed medical history, including past breast biopsies, family history of breast cancer, and any previous breast abnormalities, can provide valuable context for the evaluation. The physical examination allows for the assessment of breast symmetry, the presence of any palpable masses or skin changes, and the overall consistency of the breast tissue.
These findings, when combined with the imaging results, help to refine the differential diagnosis and identify potential risk factors.
Differential Diagnosis
Differential diagnosis of a radial scar involves distinguishing it from other breast lesions, including malignancies. Features like the lesion’s shape, margins, and internal architecture, as well as the patient’s clinical history and imaging findings, are carefully evaluated. In cases of uncertainty, a biopsy may be necessary to definitively establish the diagnosis.
Diagnostic Pathway
| Step | Description |
|---|---|
| 1. Initial Clinical Evaluation | A detailed clinical history, including risk factors and symptoms, and a thorough physical breast examination are performed. |
| 2. Imaging Assessment | Mammography, ultrasound, and MRI are utilized to evaluate the lesion’s characteristics, size, shape, and relationship to surrounding tissues. |
| 3. Radiologist Review | Radiologists review the imaging results to assess the findings and determine if further investigations are necessary. |
| 4. Differential Diagnosis | A differential diagnosis is formulated based on the clinical findings and imaging results, considering both benign and malignant possibilities. |
| 5. Biopsy (if indicated) | If the imaging and clinical findings are inconclusive, a biopsy of the lesion is performed to obtain a definitive diagnosis. |
| 6. Pathological Evaluation | A pathologist examines the biopsy specimen under a microscope to determine the nature of the lesion. |
| 7. Diagnosis and Management | The final diagnosis is established, and appropriate management strategies, which may include regular follow-up, are implemented. |
Management and Prognosis of Radial Scars
Radial scars, while benign, necessitate careful management and long-term follow-up. Understanding the strategies for managing these breast abnormalities, along with the factors influencing prognosis, is crucial for patient care. This section delves into the key aspects of managing radial scars, highlighting the importance of surveillance and the factors that contribute to their development.
Management Strategies
Effective management of radial scars hinges on a multi-faceted approach. This often involves a combination of clinical surveillance, imaging, and, in some cases, biopsy. A crucial component is regular monitoring to detect any changes in the breast tissue over time.
Long-Term Follow-Up and Surveillance, Radial scars a benign breast abnormality
Proactive long-term follow-up is paramount in managing radial scars. Regular breast imaging, such as mammograms and ultrasounds, is vital to detect any signs of evolving abnormalities. The frequency of these imaging tests is tailored to individual risk factors and the specific characteristics of the radial scar. These follow-up procedures allow for early detection of any potential changes or development of malignant lesions, ensuring prompt intervention if needed.
Risk Factors Associated with Radial Scars
Various factors can increase the likelihood of developing radial scars. Age, family history of breast cancer, and hormonal influences are potential risk factors. Further research is ongoing to fully elucidate the specific mechanisms behind radial scar development, though these factors are commonly implicated. It is important to remember that radial scars are not a direct indicator of increased breast cancer risk in all cases.
Long-Term Prognosis for Individuals with Radial Scars
The long-term prognosis for individuals with radial scars is generally favorable. Radial scars are benign and rarely progress to malignancy. However, the importance of diligent surveillance cannot be overstated. Regular monitoring allows for early detection of any changes and appropriate intervention, ensuring the best possible outcome. For example, a patient with a well-defined radial scar, with no history of breast cancer and consistent imaging results, would have a favorable prognosis.
Role of Biopsy in Managing Radial Scars
Biopsy plays a critical role in the management of radial scars, particularly when there is uncertainty regarding the nature of the lesion. A biopsy provides a definitive diagnosis, confirming the benign nature of the scar or identifying any co-existing malignant lesions. The need for a biopsy is determined based on the findings from clinical examination and imaging. In situations where suspicion for malignancy exists, a biopsy is often recommended.
Radial scars, a benign breast abnormality, are often a cause for concern, but thankfully, they usually aren’t anything serious. However, it’s crucial to consider potential links to other health issues, like liver toxicity from certain supplements. If you’re taking any supplements, it’s always a good idea to research supplements and liver toxicity to understand potential risks.
Ultimately, regular check-ups with your doctor are key to ensuring your overall well-being, especially when it comes to conditions like radial scars.
The type of biopsy used will depend on the specific clinical scenario and the location of the lesion.
Impact on Patient Care
A radial scar diagnosis, while benign, can still have a significant impact on a patient’s emotional well-being. Understanding and addressing the psychological aspects of this diagnosis is crucial for providing holistic patient care. The experience of receiving a diagnosis, especially one that may raise concerns about potential malignancy, can evoke feelings of anxiety, fear, and uncertainty. It is vital to approach patient care with empathy and sensitivity.
Psychological Impact of a Radial Scar Diagnosis
Patients diagnosed with a radial scar may experience a range of psychological reactions. Fear of cancer recurrence, despite the benign nature of the condition, is common. Concerns about the appearance of the scar and its potential impact on self-image can also contribute to emotional distress. It’s important to acknowledge and validate these feelings, providing reassurance and accurate information about the condition.
Open communication and support are essential in helping patients navigate these emotions.
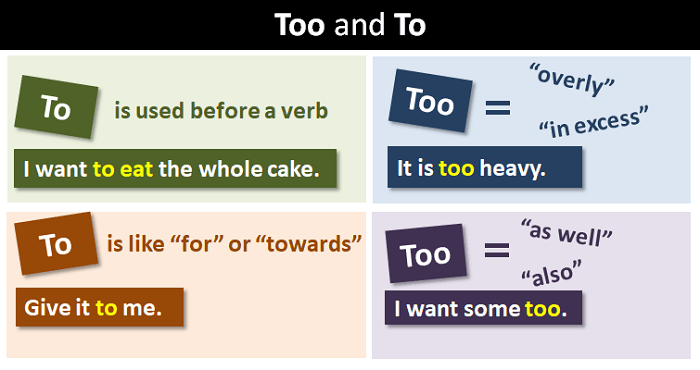
Educating Patients about Radial Scars
Clear and comprehensive education is paramount to alleviating patient anxieties and fostering understanding. This includes explaining the benign nature of radial scars, outlining their typical presentation and characteristics, and emphasizing the low risk of malignancy. Detailed information should be provided regarding the natural history of radial scars, emphasizing their tendency to remain stable over time. This approach empowers patients with knowledge, enabling them to make informed decisions about their care.
Providing visual aids, such as diagrams or images, can enhance understanding and reduce uncertainty.
Patient Communication and Shared Decision-Making
Effective communication is the cornerstone of successful patient care. Encouraging open dialogue allows patients to voice their concerns, ask questions, and actively participate in decisions about their management. This collaborative approach fosters a sense of partnership and empowers patients to take an active role in their healthcare. Shared decision-making involves actively listening to patient preferences and values, while providing evidence-based information to guide their choices.
This approach respects patient autonomy and promotes trust in the healthcare provider.
Potential Patient Questions and Answers
| Question | Answer |
|---|---|
| What is a radial scar, and why did I get one? | A radial scar is a benign breast abnormality characterized by a collection of fibrous tissue within the breast. While the exact cause isn’t always known, it often arises from previous injury or inflammation within the breast. |
| Is a radial scar cancerous? | No, radial scars are benign, meaning they are not cancerous. Although they can sometimes mimic cancerous lesions, they are not associated with an increased risk of developing breast cancer. |
| How long will my radial scar last? | Radial scars typically remain stable over time, and further growth or changes are rare. Regular monitoring by a healthcare professional is crucial for tracking any potential developments. |
| Will I need surgery for my radial scar? | Surgery is usually not necessary for radial scars unless there are concerns about their size or potential for misdiagnosis. In such cases, a biopsy may be required to confirm the diagnosis. |
| How often will I need follow-up appointments? | Follow-up appointments are determined based on individual risk factors and the healthcare provider’s recommendations. These may involve imaging studies, such as mammograms or ultrasounds, at specified intervals. |
Illustrative Cases
Radial scars, while benign, can sometimes mimic breast abnormalities, requiring careful evaluation and management. Understanding the typical presentation, imaging findings, and diagnostic approach is crucial for appropriate patient care. This section will illustrate a hypothetical case to highlight the process involved.
Hypothetical Case Presentation
A 45-year-old female patient presents with a palpable, well-defined, firm mass in her right breast. She reports no pain or nipple discharge. The patient has a history of fibrocystic breast changes and has undergone several mammograms in the past. The patient’s family history includes a history of breast cancer in her mother and an aunt.
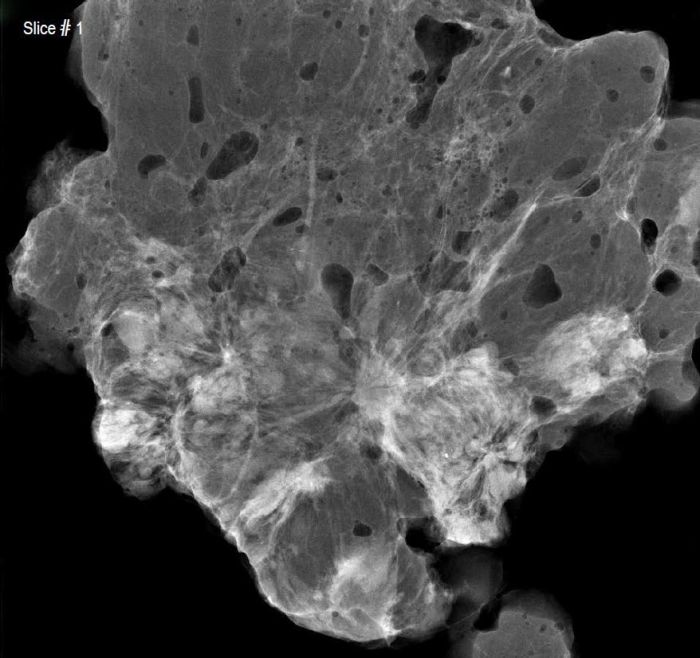
Imaging Findings
Mammogram reveals a well-circumscribed, dense area in the right breast, with no associated microcalcifications. Ultrasound demonstrates a hypoechoic mass with well-defined margins, consistent with a radial scar. Further evaluation with MRI reveals a radial scar with a prominent central core and radiating fibrous bands. The MRI findings provide crucial details for distinguishing the scar from other breast lesions.
Diagnostic Approach and Management Plan
Given the patient’s history, physical exam, and imaging findings, a definitive diagnosis of radial scar is considered. The patient undergoes a core needle biopsy to confirm the diagnosis. The pathology report confirms the presence of a radial scar. The multidisciplinary approach is critical in determining the best course of action. A breast surgeon, radiologist, and pathologist will collaborate to discuss the appropriate management plan.
Multidisciplinary Care in Management
A multidisciplinary team approach is essential for optimal patient care in cases of suspected radial scar. The team considers the patient’s age, family history, and other risk factors. The goal is to avoid unnecessary biopsies or surgeries while ensuring that all suspicious findings are thoroughly investigated. This collaborative approach facilitates shared decision-making and minimizes the potential for misdiagnosis.
The team thoroughly discusses the benefits and risks of various management options.
Case Study
| Patient Information | Physical Exam | Imaging Findings | Diagnosis |
|---|---|---|---|
| 45-year-old female, history of fibrocystic breast changes, family history of breast cancer | Palpable, well-defined, firm mass in the right breast, no pain or nipple discharge | Mammogram: well-circumscribed dense area, no microcalcifications; Ultrasound: hypoechoic mass with well-defined margins; MRI: radial scar with prominent central core and radiating fibrous bands | Radial Scar |
The case highlights the importance of a comprehensive approach to diagnosing and managing radial scars. A thorough evaluation, including patient history, physical examination, and imaging studies, is critical for accurate diagnosis. Collaboration among specialists is essential to determine the appropriate management strategy, minimizing the risk of unnecessary interventions.
Future Research Directions
Radial scars, while benign, present ongoing challenges in diagnosis and management. Understanding their natural history, particularly in long-term follow-up, is crucial for improving patient care. Further research into these benign breast lesions is vital to refine diagnostic criteria, tailor management strategies, and ultimately alleviate patient anxiety and uncertainty.
Natural History and Long-Term Follow-up
Understanding the natural progression of radial scars over extended periods is essential. Studies focusing on long-term follow-up, including imaging assessments and clinical evaluations, can provide valuable insights into the stability and potential for any morphological changes in radial scars. This will allow for a more precise understanding of their natural behavior, which is currently limited. Collecting data on a large cohort of patients with radial scars over many years is crucial for developing reliable predictions regarding their future behavior.
Development of Enhanced Diagnostic Tools
Current diagnostic modalities, while helpful, can sometimes be inconclusive. Further research into the development of more specific and sensitive diagnostic tools, such as advanced imaging techniques (e.g., contrast-enhanced MRI with specific protocols) and novel biomarker analysis, is needed. This could potentially differentiate radial scars from other breast pathologies with greater accuracy, reducing unnecessary biopsies and improving patient management.
Refinement of Management Strategies
While current management strategies are generally conservative, further research can refine these approaches. Investigating the effectiveness of various surveillance protocols, tailored to the individual characteristics of the radial scar, could potentially optimize patient care. Studies evaluating the impact of different surveillance intervals and imaging modalities on patient outcomes are essential. This would involve considering factors such as the size, location, and appearance of the radial scar on imaging.
Application of Artificial Intelligence (AI) in Diagnosis
AI algorithms have demonstrated promising potential in various medical fields, and their application in breast imaging is no exception. Further research into the use of AI for the automated detection and characterization of radial scars on mammograms and ultrasound images could significantly improve diagnostic efficiency and accuracy. This could potentially reduce the workload on radiologists and expedite the diagnosis process.
Examples of AI-powered diagnostic systems already in development can be applied to this area, and their performance can be evaluated using large datasets of radial scar cases.
The Role of Biomarkers
Identifying specific biomarkers associated with radial scars could revolutionize diagnostic approaches. Research focused on discovering and validating such biomarkers could enhance the accuracy of differential diagnosis and aid in predicting the natural history of the lesion. These markers could be analyzed through blood tests, tissue biopsies, or imaging techniques. This approach would enable a more targeted and personalized approach to patient management.
Summary
In conclusion, radial scars, while benign, can sometimes present challenges in diagnosis due to their potential to mimic malignant breast lesions. A thorough understanding of their characteristics, imaging findings, and diagnostic procedures is essential for accurate assessment and appropriate management. Open communication, shared decision-making, and patient education play a crucial role in providing the best possible care for individuals with radial scars.
Further research and advancements in diagnostic techniques hold promise for improving the accuracy and efficiency of identifying and managing these abnormalities.