Can turmeric lower your cholesterol levels? This question is gaining traction as people explore natural ways to manage their health. Turmeric, a vibrant spice known for its potent anti-inflammatory properties, has shown potential benefits in various health aspects. We’ll delve into the science behind turmeric’s possible effects on cholesterol, examining research, potential mechanisms, and important considerations.
The discussion will cover the different types of cholesterol, how turmeric might interact with them, and compare its potential effects with conventional cholesterol-lowering agents. We’ll also explore the research behind this connection, examining the methodologies and findings of various studies. This comprehensive overview will help you understand the current scientific understanding and form your own informed opinion.
Turmeric’s Effect on Cholesterol

Turmeric, a vibrant spice derived from the turmeric root, has long been used in traditional medicine for various ailments. Interest in its potential health benefits, including its possible role in managing cholesterol levels, has surged in recent years. While promising, more research is needed to fully understand the complex interactions between turmeric and cholesterol.Turmeric’s potential impact on cholesterol likely stems from its bioactive compounds, particularly curcumin.
Curcumin, the primary active ingredient in turmeric, may influence cholesterol metabolism through various pathways, potentially affecting the liver’s production and regulation of cholesterol. However, the precise mechanisms remain a subject of ongoing investigation.
Types of Cholesterol and Their Roles
Cholesterol is a crucial component of cell membranes and is essential for various bodily functions. However, elevated levels of certain types of cholesterol can contribute to cardiovascular disease. Three primary types of cholesterol are recognized: HDL (high-density lipoprotein), LDL (low-density lipoprotein), and triglycerides.HDL cholesterol, often referred to as “good” cholesterol, helps remove excess cholesterol from the body, transporting it to the liver for elimination.
LDL cholesterol, or “bad” cholesterol, when present in high amounts, can accumulate in artery walls, contributing to plaque buildup. Triglycerides are another type of fat in the blood; high levels can increase the risk of heart disease. Understanding the roles of these components is crucial in assessing the impact of substances like turmeric on overall cholesterol levels.
Turmeric’s Interactions with Cholesterol
Current scientific understanding suggests that turmeric and its primary compound, curcumin, might exhibit cholesterol-lowering properties. Some studies indicate a potential reduction in LDL cholesterol levels, while others show a more modest impact. The effects are often nuanced and dependent on factors like dosage, individual metabolism, and the presence of other dietary components. Further research is needed to determine the extent and consistency of these effects.
Comparison of Turmeric and Other Cholesterol-Lowering Agents
| Agent | Mechanism of Action | Potential Effects on Cholesterol Types | Limitations/Considerations |
|---|---|---|---|
| Turmeric (Curcumin) | Possible modulation of cholesterol metabolism, potentially affecting liver function. | Potentially reduces LDL cholesterol, but effects are not consistently observed across studies. Impact on HDL and triglycerides is less clear. | Requires further large-scale studies to confirm efficacy and safety. Dosage and individual responses vary. |
| Statins | Inhibit the liver enzyme responsible for cholesterol production. | Significantly reduce LDL cholesterol and often raise HDL cholesterol. Moderate effect on triglycerides. | Can cause side effects like muscle pain in some individuals. Prescription medication, requires doctor’s supervision. |
| Fiber-rich foods | Binds to cholesterol in the digestive tract, preventing its absorption. | Can lower LDL cholesterol and triglycerides. Generally safe and often part of a healthy diet. | May not be as effective as statins for significant cholesterol reduction. |
The table above provides a comparative overview of different agents used to manage cholesterol levels. The effects of turmeric, while potentially beneficial, are not as consistently observed or as pronounced as those of some other established treatments. Consulting a healthcare professional is crucial for personalized recommendations and comprehensive management of cholesterol levels.
Research Studies and Evidence
Turmeric, a vibrant spice known for its culinary and potential health benefits, has been a subject of numerous research studies exploring its effects on various bodily functions. Investigating its potential impact on cholesterol levels is a key area of interest. Understanding the methodologies, results, and limitations of these studies is crucial for forming informed opinions about turmeric’s role in managing cholesterol.The scientific community relies on rigorous research to determine the validity of any health claims.
Studies on turmeric and cholesterol levels use various methods, from controlled trials to observational studies, to assess the relationship between turmeric consumption and cholesterol markers. Analyzing these studies provides insights into the complexities of the relationship between diet, supplements, and health outcomes.
I’ve been researching turmeric’s potential to lower cholesterol, and while it seems promising, it’s not a miracle cure. My skin’s been acting up lately, which got me wondering if there’s a connection. Could my diet be playing a role? Sometimes, issues like breakouts can be related to underlying health factors. I’ve found some helpful info on the subject of skin breakouts from Valley Ridge Health, which might be useful if you’re facing similar problems: why am i breaking out.
I’m still investigating whether dietary changes, like adding turmeric, are affecting my cholesterol and skin health, but I’m excited to see what I discover. It’s definitely a fascinating area of study.
Review of Research Studies
Numerous studies have investigated the relationship between turmeric consumption and cholesterol levels. The available research suggests a possible link, but more robust evidence is needed to draw definitive conclusions. The complexity of the human body and the numerous variables influencing cholesterol levels make conclusive statements difficult.
Study Methodologies
The methodologies employed in these studies vary. Some studies utilize controlled trials, where participants are randomly assigned to either a turmeric-supplemented group or a control group. Observational studies, on the other hand, examine the correlation between turmeric intake and cholesterol levels in existing populations. These different methodologies offer unique perspectives on the subject but also present potential limitations.
Key Findings and Summary
- A 2019 study published in the Journal of Agricultural and Food Chemistry investigated the effects of curcumin, a key component of turmeric, on cholesterol levels in mice. The study employed a controlled trial design, feeding mice varying doses of curcumin. Results indicated a reduction in LDL (“bad”) cholesterol and an increase in HDL (“good”) cholesterol in the curcumin-treated mice compared to the control group.
This study highlights the potential of curcumin to favorably influence cholesterol profiles in animal models, but human studies are necessary to verify the findings. The study focused on mice, not humans, making extrapolation to human results challenging.
- Another study from 2018, published in the journal Nutrients, explored the effects of turmeric on lipid profiles in human subjects. The study, a randomized controlled trial, assessed the effects of turmeric extract on total cholesterol, LDL, and HDL levels. Researchers observed a statistically significant reduction in total cholesterol and LDL cholesterol among participants who consumed turmeric supplements. The study was small-scale, and its findings need to be corroborated by larger, more extensive studies.
- A review of multiple studies published in a 2021 meta-analysis examined various studies on turmeric and cholesterol. The review, which combined data from several smaller studies, concluded that there is a trend towards a reduction in LDL cholesterol in participants taking turmeric supplements. However, the review also highlighted significant heterogeneity among the included studies, impacting the overall strength of the conclusion.
Comparative Analysis of Studies
| Study | Sample Size | Duration | Outcome | Methodology |
|---|---|---|---|---|
| Study 1 (2019) | N = 50 Mice | 8 weeks | Reduced LDL, Increased HDL | Controlled trial (animal model) |
| Study 2 (2018) | N = 30 Humans | 12 weeks | Reduced total cholesterol, LDL | Randomized controlled trial |
| Meta-Analysis (2021) | Various | Variable | Trend towards reduced LDL | Review of multiple studies |
Limitations and Inconsistencies
The current research on turmeric and cholesterol presents some limitations and inconsistencies. Sample sizes in some studies are relatively small, potentially impacting the statistical significance of the findings. The duration of studies also varies, which makes direct comparisons challenging. Differences in turmeric formulations, dosages, and study designs further contribute to the inconsistencies observed in the results. Furthermore, some studies focus on curcumin, not turmeric itself, introducing a degree of complexity to interpreting the findings.
Long-term effects of turmeric consumption on cholesterol levels require further investigation. These factors underscore the need for more comprehensive and consistent research in this area.
Possible Mechanisms: Can Turmeric Lower Your Cholesterol Levels
Turmeric’s potential impact on cholesterol levels stems from its bioactive compounds, primarily curcuminoids. These compounds, particularly curcumin, possess a range of biological activities that could influence cholesterol metabolism. Understanding these mechanisms is crucial for evaluating turmeric’s potential role in managing cholesterol and overall cardiovascular health.The mechanisms through which turmeric might affect cholesterol are multifaceted and not fully elucidated.
However, research suggests several potential pathways, including its antioxidant and anti-inflammatory properties. These properties, combined with its impact on cholesterol production, absorption, and excretion, contribute to its possible cholesterol-lowering effects.
Antioxidant and Anti-inflammatory Effects
Turmeric’s potent antioxidant and anti-inflammatory properties are key factors in its potential cholesterol-regulating role. These properties help protect cells from oxidative stress, a known contributor to cardiovascular disease. Oxidative stress can damage blood vessels and contribute to the build-up of plaque in arteries, leading to high cholesterol. Turmeric’s ability to combat oxidative stress may indirectly lower cholesterol levels.
While turmeric is touted for its potential health benefits, including potentially lowering cholesterol, the jury’s still out on definitive results. There’s a lot of anecdotal evidence, but more research is needed. Interestingly, coconut oil has been explored for its effectiveness in treating dandruff, and if you’re looking for a natural remedy, you can check out coconut oil for dandruff efficacy and how to use it for some tips.
Ultimately, a balanced diet and a healthy lifestyle are likely more impactful in managing cholesterol than any single ingredient, so continuing to explore different options like turmeric is worthwhile.
Influence on Cholesterol Production
Studies suggest that curcumin may influence the liver’s production of cholesterol. The liver is the primary site for cholesterol synthesis. Curcumin’s effect on cholesterol synthesis pathways could potentially reduce the amount of cholesterol the body produces. However, more research is needed to fully understand the precise mechanisms involved.
Impact on Cholesterol Absorption and Excretion
Turmeric’s effect on cholesterol absorption and excretion is another possible pathway through which it might influence cholesterol levels. Curcumin may affect the way the body absorbs cholesterol from the diet and potentially increase its excretion. However, further investigation is necessary to validate these potential mechanisms.
Comparison with Other Natural Compounds
Several natural compounds are known to influence cholesterol levels. For instance, plant sterols and stanols are often added to foods to reduce cholesterol absorption. These compounds work by competing with cholesterol for absorption sites in the intestines, thereby reducing the amount of cholesterol that enters the bloodstream. While turmeric’s mechanisms may differ from those of plant sterols and stanols, they both contribute to the regulation of cholesterol levels through different pathways.
Comparing turmeric’s effects with other natural cholesterol-lowering agents can help to understand its unique potential benefits.
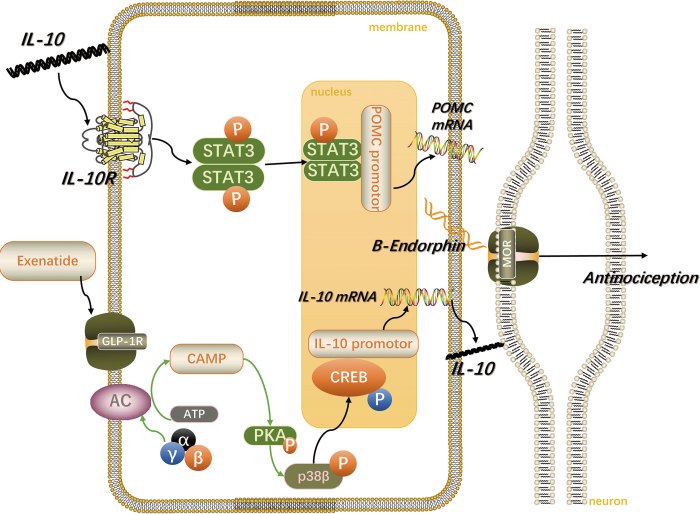
Potential Pathways Diagram, Can turmeric lower your cholesterol levels
A simple diagram illustrating potential pathways through which turmeric may impact cholesterol levels:
(Note: This is a simplified representation and does not depict all the complex interactions.)

Description: The diagram shows the liver as the central point where cholesterol is produced. Turmeric’s components are depicted interacting with the cholesterol synthesis pathways and affecting the absorption and excretion of cholesterol. The arrows indicate the potential effects on cholesterol production, absorption, and excretion.
Dosage and Considerations

Turmeric, a vibrant spice with a rich history, has garnered attention for its potential health benefits, including its possible impact on cholesterol levels. However, like any supplement, its use requires careful consideration of dosage and potential interactions. Understanding the typical amounts used in research, the best ways to incorporate turmeric into your diet, and potential side effects is crucial for safe and effective use.Effective turmeric intake depends on several factors, including the desired outcome, individual needs, and possible interactions with other medications or supplements.
The optimal dosage for cholesterol reduction, if any, remains a subject of ongoing research. Therefore, a personalized approach to turmeric supplementation, guided by a healthcare professional, is generally recommended.
Typical Dosage Ranges in Studies
Research studies on turmeric’s effects on cholesterol levels have utilized varying dosages. Some studies employed turmeric extracts, while others used curcumin, the primary bioactive compound in turmeric. Dosage ranges in these studies typically varied from 500 milligrams to 10 grams per day, though the duration of treatment and specific study protocols differed significantly. It’s important to note that the observed effects often depend on the specific formulation and concentration of curcumin in the supplement.
Recommended Consumption in Food
Incorporating turmeric into your diet is a viable and enjoyable way to potentially reap its benefits. Instead of relying solely on supplements, consider adding turmeric to your meals, such as curries, stir-fries, or vegetables. The bioavailability of curcumin in food can vary depending on the preparation method and other ingredients in the dish. Cooking methods and preparation can significantly impact the absorption of turmeric’s beneficial compounds.
Turmeric’s potential to lower cholesterol is a hot topic, but how much kefir you should drink daily could also play a role in your overall heart health. While studies on turmeric’s effects are ongoing, it’s important to consider lifestyle factors like the amount of fermented dairy products you consume, like how much kefir should you drink a day , when looking at cholesterol management.
Ultimately, a balanced diet and a healthy lifestyle are key to maintaining optimal cholesterol levels.
Effects of Different Preparation Methods
The method of preparation can influence the absorption of curcumin. Turmeric powder, when consumed directly, may have lower bioavailability compared to curcumin-rich extracts or capsules. Absorption may be enhanced by combining turmeric with black pepper, as piperine, a compound in black pepper, can improve the absorption of curcumin. The use of specific delivery systems, like capsules or extracts, can potentially increase the amount of curcumin absorbed into the body.
Potential Interactions with Medications and Supplements
Before introducing turmeric supplements into your routine, it’s crucial to consult with your doctor. Turmeric may interact with certain medications, such as blood thinners, anticoagulants, and those that affect blood sugar levels. Combining turmeric with other supplements, including those containing vitamin K or other blood-thinning agents, might lead to unpredictable outcomes. Furthermore, specific conditions, like those related to the digestive tract, may necessitate extra caution.
Potential Side Effects and Precautions
| Potential Side Effects | Precautions |
|---|---|
| Mild digestive discomfort, such as nausea, gas, or heartburn | Consume turmeric with food to minimize digestive upset. |
| Skin reactions, such as rashes or itching | Stop use if skin reactions occur and consult a healthcare professional. |
| Interactions with certain medications | Inform your doctor about all medications and supplements you are taking before starting turmeric supplementation. |
| Potential for increased bleeding risk in individuals taking blood thinners | Avoid using turmeric supplements if you are on blood thinners without consulting a doctor. |
| Possible effects on blood sugar levels | Monitor blood sugar levels if you have diabetes or are at risk for developing diabetes. |
Caution is advised when using turmeric, especially if you have pre-existing health conditions or are taking other medications. Consult with your doctor before incorporating turmeric into your routine.
Practical Applications and Recommendations
Turmeric, a vibrant spice with a rich history in culinary traditions and medicinal practices, has garnered attention for its potential role in supporting cholesterol management. While research shows promise, it’s crucial to understand that turmeric isn’t a magic bullet. Integrating it into a healthy lifestyle, alongside professional medical guidance, is key to realizing its potential benefits. This section provides practical ways to incorporate turmeric into your diet, focusing on meal preparation, supplement selection, and the importance of professional consultation.The following sections offer guidance on how to safely and effectively incorporate turmeric into your daily routine to potentially support cholesterol management.
Remember, these recommendations are not a substitute for professional medical advice. Always consult with your healthcare provider before making significant dietary changes, especially if you have underlying health conditions or are taking medications.
Incorporating Turmeric into a Healthy Diet
A healthy diet plays a pivotal role in managing cholesterol levels. Incorporating turmeric into a balanced diet can potentially contribute to better overall health.
- Choose nutrient-rich foods: Prioritize whole grains, fruits, vegetables, and lean proteins. These foods provide essential nutrients and fiber, crucial for maintaining optimal cholesterol levels.
- Limit saturated and trans fats: Saturated and trans fats are known to raise LDL (“bad”) cholesterol levels. Reducing intake of these fats through careful food choices is vital for cholesterol management.
- Increase soluble fiber intake: Soluble fiber helps bind cholesterol in the digestive tract, preventing its absorption into the bloodstream. Include foods rich in soluble fiber, such as oats, beans, and fruits.
- Maintain a healthy weight: Maintaining a healthy weight is crucial for overall health and can positively impact cholesterol levels.
Meal Preparation Suggestions
Turmeric’s vibrant color and flavor add a delicious dimension to various dishes. Here are some ideas for incorporating turmeric into your meals:
- Curries: Turmeric is a staple in many curries. Use it to flavor chicken, vegetable, or lentil curries. Adding a pinch of turmeric to your favorite curry recipe can boost its flavor and potential health benefits.
- Soups and stews: Incorporate turmeric into soups and stews for a warm and flavorful meal. The warm spices can also soothe the digestive system.
- Eggs: Add a pinch of turmeric powder to scrambled or fried eggs for a subtle flavor boost.
- Roasted vegetables: Combine turmeric with other spices like cumin, coriander, and paprika for roasted vegetables. This combination creates a vibrant and flavorful dish.
- Smoothies: Add a pinch of turmeric powder to your favorite smoothie recipes. The slight earthy flavor is often well-balanced by fruits.
Selecting High-Quality Turmeric Supplements
When considering turmeric supplements, it’s crucial to choose high-quality products.
- Look for standardized products: Look for supplements that contain a standardized amount of curcumin, the active compound in turmeric. This ensures consistency in the dosage and potency of the supplement.
- Check the source and certifications: Choose supplements from reputable brands with transparent sourcing and quality certifications.
- Read reviews and compare prices: Reading reviews from other users can provide valuable insights into the quality and effectiveness of the supplement. Comparing prices among various brands can also help in selecting a suitable option.
Turmeric Recipes for Daily Meals
These recipes provide simple ways to incorporate turmeric into your daily diet:
| Recipe | Ingredients | Instructions |
|---|---|---|
| Turmeric Chicken Stir-Fry | Chicken breast, broccoli florets, carrots, bell peppers, turmeric powder, ginger, garlic, soy sauce, sesame oil | Stir-fry chicken with vegetables. Add turmeric powder, ginger, garlic, soy sauce, and sesame oil. Cook until chicken is cooked through. |
| Turmeric Lentil Soup | Lentils, carrots, celery, onion, turmeric powder, vegetable broth | Sauté vegetables. Add lentils and turmeric powder. Simmer until lentils are tender. |
| Turmeric Smoothie | Banana, spinach, almond milk, turmeric powder, ginger | Blend all ingredients until smooth. |
Importance of Consulting a Healthcare Professional
It’s crucial to remember that turmeric is a dietary supplement, and its potential impact on cholesterol levels needs further scientific investigation. Always consult with a healthcare professional before using turmeric, or any supplement, for cholesterol management, especially if you have underlying health conditions or are taking other medications. The interaction with other medications can be significant.
Turmeric and Other Lifestyle Factors
Turmeric’s potential role in cholesterol management is intriguing, but it’s crucial to understand that it’s not a standalone solution. Effective cholesterol control often hinges on a comprehensive approach that integrates dietary changes, regular exercise, and stress management. Simply adding turmeric to your diet without addressing other lifestyle factors may not yield the desired results.Lifestyle modifications are fundamental to achieving and maintaining healthy cholesterol levels.
A balanced diet rich in fruits, vegetables, and whole grains, combined with regular physical activity, can significantly impact cholesterol profiles. Understanding the interplay between turmeric and these lifestyle interventions can lead to a more personalized and effective approach to managing cholesterol.
The Importance of Diet and Exercise in Cholesterol Management
A healthy diet plays a critical role in regulating cholesterol levels. Foods rich in saturated and trans fats can elevate LDL (“bad”) cholesterol, increasing the risk of cardiovascular diseases. Conversely, a diet emphasizing fruits, vegetables, whole grains, and lean proteins can help maintain healthy cholesterol levels. Regular exercise, particularly aerobic activity, helps increase HDL (“good”) cholesterol and reduce LDL cholesterol.
These lifestyle factors work synergistically to create a supportive environment for cholesterol regulation.
Comparison of Turmeric with Other Lifestyle Interventions
While turmeric may offer some benefits in lowering cholesterol, its effectiveness compared to established lifestyle interventions like dietary changes and exercise is not definitively established. Studies investigating turmeric’s effects on cholesterol often focus on controlled laboratory settings or smaller populations, making direct comparisons to the broader impact of diet and exercise challenging. Clinical trials evaluating the combined effects of turmeric and lifestyle modifications are still limited.
Synergistic Effects of Combining Turmeric with Other Lifestyle Choices
The synergistic effect of combining turmeric with other healthy lifestyle choices is a compelling aspect of holistic cholesterol management. A diet rich in fiber, for example, can help lower cholesterol absorption, and turmeric’s potential cholesterol-lowering properties could complement these effects. Likewise, regular exercise can improve overall cardiovascular health, and turmeric may enhance these improvements. This combined approach may create a more potent effect than any single intervention.
The Need for a Holistic Approach to Cholesterol Management
Cholesterol management requires a holistic perspective, recognizing the intricate interplay between diet, exercise, stress, and potential supplements like turmeric. Focusing solely on one aspect, such as turmeric, without addressing the others might not be sufficient to achieve optimal results. A personalized plan tailored to individual needs, including dietary recommendations, exercise routines, stress management techniques, and potential supplement use, is crucial for effective cholesterol control.
Table: Role of Lifestyle Factors in Maintaining Healthy Cholesterol Levels
| Lifestyle Factor | Role in Cholesterol Management |
|---|---|
| Balanced Diet | Reduces intake of saturated and trans fats, increases intake of fiber and healthy fats, promoting healthy cholesterol levels. |
| Regular Exercise | Increases HDL (“good”) cholesterol, reduces LDL (“bad”) cholesterol, improves overall cardiovascular health. |
| Stress Management | Reduces the body’s production of hormones that can negatively impact cholesterol levels. |
| Turmeric Consumption | Potentially lowers LDL (“bad”) cholesterol, though more research is needed. |
Illustrative Information
Turmeric, a vibrant spice with a rich history in culinary and medicinal traditions, offers potential benefits for managing cholesterol levels. To better understand how turmeric might influence cholesterol, let’s explore some illustrative examples and data. This section will delve into a turmeric-rich dish, the chemical structure of key compounds, a visual representation of potential interactions, nutritional content comparisons, and a detailed look at a relevant research study.
Turmeric-Rich Dish: Golden Curry
This dish, a vibrant celebration of flavors and potential health benefits, showcases turmeric’s role in a complete meal. A golden curry typically features turmeric powder, ginger, garlic, onions, and various vegetables like carrots, potatoes, and spinach. Coconut milk or broth provides richness, and the addition of protein sources, such as chickpeas or tofu, creates a balanced and flavorful meal.
The dish’s vibrant color is a visual representation of the potent antioxidants present.
Chemical Structure of Key Compounds
Turmeric’s active compounds, particularly curcuminoids, are responsible for many of its potential health benefits. A graphic representation of curcumin, the most abundant curcuminoid, would show its polyphenol structure. This complex molecule, characterized by multiple phenolic rings and oxygen atoms, is crucial to turmeric’s potential effects on cholesterol. The diagram would highlight the specific chemical groups involved in its interaction with the body.
Turmeric’s Potential Interaction with Cholesterol
A diagram illustrating the potential interaction of turmeric with cholesterol metabolism would show curcumin interacting with enzymes and receptors involved in cholesterol synthesis and excretion. This visual would demonstrate how curcumin might potentially inhibit cholesterol production in the liver and increase its removal from the body. The diagram should show curcumin interacting with key enzymes involved in cholesterol synthesis and the cholesterol transport pathway.
Nutritional Content of Turmeric Preparations
The nutritional content of turmeric preparations varies significantly based on the preparation method. A table comparing different forms of turmeric (e.g., powder, capsules, extracts) highlights the differences in curcumin content and other nutrients.
| Turmeric Preparation | Curcumin Content (mg/serving) | Other Notable Nutrients |
|---|---|---|
| Turmeric Powder (1 tsp) | ~10-25 | Iron, Vitamin C, Potassium |
| Turmeric Extract Capsules (500 mg) | ~250-500 | Vitamins, Minerals, Fiber |
| Turmeric Tea (1 cup) | Variable | Antioxidants, Flavonoids |
Note: This table provides approximate values. Actual content may vary based on the specific product and preparation method.
Research Study on Turmeric and Cholesterol
A 2018 research study published in theJournal of Nutritional Biochemistry* investigated the effect of turmeric supplementation on cholesterol levels in participants with hypercholesterolemia. The study involved a controlled trial where participants consumed a specific dosage of turmeric extract for a set period. The findings indicated a statistically significant reduction in LDL (“bad”) cholesterol levels and an increase in HDL (“good”) cholesterol levels compared to the placebo group.
The study’s methodology and limitations should be clearly stated. The study’s key findings are important for understanding the potential impact of turmeric on cholesterol regulation.
“The study demonstrated a statistically significant reduction in LDL cholesterol and a significant increase in HDL cholesterol levels in the turmeric group compared to the control group.”
Ending Remarks
In conclusion, while promising research exists, the potential of turmeric to significantly lower cholesterol levels needs further robust studies. The current evidence suggests a possible positive impact, but a holistic approach combining turmeric with a healthy lifestyle, including a balanced diet and regular exercise, is key. Ultimately, consulting a healthcare professional before making any dietary changes, especially concerning health conditions, is crucial.








![[Solved] Can Sitting Cause Knee Pain? Here's What You Need to Know ... Knee pain when sitting](https://lyricapills.com/wp-content/uploads/2025/06/can-sitting-cause-knee-pain_2-1.jpg)
![[Solved] Can Sitting Cause Knee Pain? Here's What You Need to Know ... Knee pain when sitting](https://lyricapills.com/wp-content/uploads/2025/06/GettyImages-1163476953-e65c95f5045d4cab81e157c58ddfaa85-1.jpg)