Tioconazole vs miconazole what are the differences? This deep dive explores the nuances between these two antifungal medications. We’ll examine their mechanisms of action, available forms, dosages, potential side effects, and more. Understanding these differences is crucial for informed discussions with healthcare professionals and for making the best treatment decisions for fungal infections.
Both tioconazole and miconazole are commonly used to treat various fungal infections, but their specific characteristics and applications can vary. This comparison aims to provide a comprehensive overview, enabling a clearer understanding of their individual strengths and weaknesses.
Introduction to Antifungal Medications
Antifungal medications are a crucial class of drugs used to combat fungal infections, a diverse range of illnesses that affect various parts of the body. These infections can range from superficial skin conditions to systemic diseases, impacting individuals of all ages and backgrounds. Understanding the mechanisms of action and types of fungal infections these medications target is essential for effective treatment and patient care.These medications work by interfering with the growth and development of fungal cells.
This often involves targeting specific metabolic processes unique to fungi, while minimizing harm to human cells. Their role is pivotal in controlling and eradicating fungal infections, preventing complications and promoting overall health. Different types of fungal infections require specific antifungal treatments tailored to the particular fungal species and the site of the infection.
Common Types of Fungal Infections
Fungal infections, also known as mycoses, can affect various parts of the body, leading to diverse symptoms. Superficial infections, such as athlete’s foot and ringworm, commonly involve the skin, hair, and nails. Other types, like candidiasis, can affect mucous membranes and deeper tissues. Systemic mycoses, such as histoplasmosis and aspergillosis, are more severe and can spread throughout the body.
Prompt diagnosis and appropriate treatment are essential to managing these infections effectively.
Mechanisms of Action of Antifungal Medications
Antifungal medications employ various strategies to inhibit fungal growth. Some medications interfere with the synthesis of fungal cell walls, while others disrupt the production of ergosterol, a crucial component of fungal cell membranes. Still others target the synthesis of nucleic acids or other essential metabolic processes. Understanding the specific mechanisms of action of each medication is crucial for determining the best treatment strategy for a particular fungal infection.
Comparison of Antifungal Medications
| Medication Type | Target Fungal Infections | Routes of Administration |
|---|---|---|
| Azoles (e.g., fluconazole, clotrimazole) | Yeast infections, dermatophytes (ringworm), some molds | Oral, topical, vaginal |
| Allylamines (e.g., terbinafine) | Dermatophytes (ringworm, athlete’s foot) | Oral, topical |
| Polyenes (e.g., amphotericin B) | Systemic fungal infections, particularly severe cases | Intravenous (IV), topical |
| Echinocandins (e.g., caspofungin) | Yeast infections, particularly invasive candidiasis | Intravenous (IV) |
| Imidazoles (e.g., miconazole, tioconazole) | Superficial fungal infections, such as skin infections and yeast infections | Topical, vaginal |
This table provides a general overview of common antifungal medications, their targeted infections, and typical administration routes. The specific choice of medication depends on the type of infection, its severity, and the patient’s overall health. Careful consideration of these factors is crucial for optimal treatment outcomes.
Tioconazole Overview
Tioconazole is a commonly prescribed antifungal medication, primarily used to treat various superficial fungal infections. Its effectiveness stems from its unique mechanism of action, which targets the fungal cell membrane. Understanding its diverse formulations and appropriate dosages is crucial for optimal treatment outcomes.
Mechanism of Action
Tioconazole disrupts the fungal cell membrane by interacting with ergosterol, a crucial component of the fungal cell membrane. This interaction leads to the leakage of essential intracellular components, ultimately inhibiting fungal growth and reproduction. The precise molecular mechanisms involved in this process are still under active investigation, but the overall outcome is clear: Tioconazole effectively targets and eliminates fungal pathogens.
I’ve been researching tioconazole vs. miconazole lately, trying to figure out which antifungal works best. While researching, I stumbled upon a fascinating article about the effectiveness of pore strips. Have you ever wondered if those things actually do anything? If you’re curious about their efficacy, check out this informative piece on do pore strips work.
Ultimately, though, my main focus is still on the key differences between tioconazole and miconazole for fungal infections. I’m still trying to nail down the best option for my needs.
Available Forms
Tioconazole is available in various topical formulations to address different infection sites and patient preferences. These formulations are designed to deliver the medication directly to the affected area, maximizing its therapeutic effect and minimizing systemic exposure.
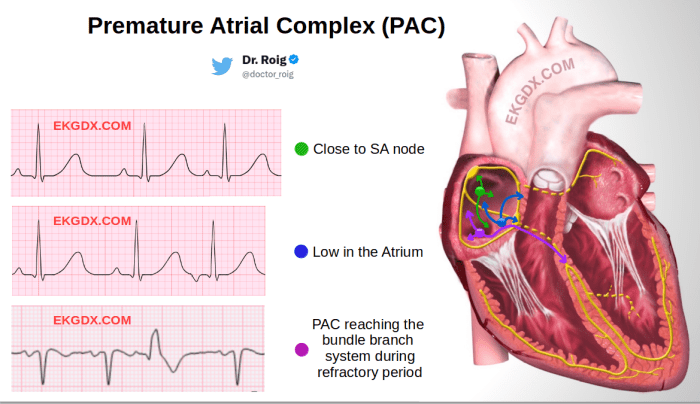
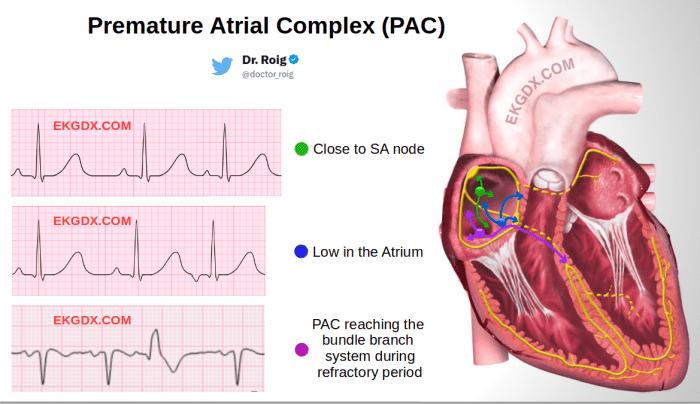
So, you’re looking at tioconazole vs miconazole? They’re both antifungal medications, but subtle differences exist. While these differences are important for treating fungal infections, it’s crucial to remember that they are not related to conditions like premature atrial complexes PACs, which are a type of arrhythmia. Understanding the nuances of these medications, such as their absorption rates and potential side effects, is key for effective treatment.
For more information on premature atrial complexes PACs, check out this helpful resource: premature atrial complexes pacs. Ultimately, the best choice between tioconazole and miconazole will depend on your specific needs and the advice of your healthcare provider.
- Creams: Tioconazole creams are typically used for treating skin infections, offering a smooth and easy application method. The cream formulation allows for better penetration of the medication into the skin layers, facilitating the treatment of deeper fungal infections.
- Ointments: Tioconazole ointments are another topical form, often preferred for their thicker consistency. This thicker texture can be beneficial for areas with significant skin irritation or inflammation, helping to soothe and protect the affected area while delivering the medication effectively.
- Powders: Tioconazole powders are a useful formulation for treating fungal infections in intertriginous areas (skin folds), like the groin or underarms. Their ability to absorb moisture helps maintain a dry environment, which is crucial for inhibiting fungal growth.
Dosage and Administration
Appropriate dosage and administration guidelines are critical for maximizing the effectiveness of tioconazole and minimizing potential side effects. These guidelines vary based on the specific formulation and the severity of the infection. Always consult a healthcare professional for personalized recommendations.
Table of Tioconazole Formulations
| Formulation | Strength (mg/g) | Typical Application |
|---|---|---|
| Cream | 1% | Twice daily, for 2-4 weeks |
| Ointment | 1% | Twice daily, for 2-4 weeks |
| Powder | 1% | Apply liberally to affected area, 2-3 times daily, as needed |
Miconazole Overview
Miconazole is a widely used antifungal medication, effectively combating various fungal infections. Its diverse applications and proven efficacy make it a crucial component in dermatological and even systemic treatments. Understanding its mechanism of action, available forms, and appropriate dosage is essential for its safe and effective use.
Mechanism of Action
Miconazole functions by disrupting the fungal cell membrane’s integrity. It achieves this by inhibiting ergosterol synthesis, a crucial component of the fungal cell membrane. By interfering with this process, miconazole prevents the formation of a stable and functional membrane, ultimately leading to fungal cell death. This mechanism of action makes it effective against a range of fungal pathogens.
Available Forms
Miconazole is available in various forms, catering to different types of fungal infections and patient needs. These diverse formulations ensure appropriate delivery and treatment effectiveness.
- Topical Applications: Miconazole is commonly formulated as creams, ointments, and powders for topical application to the skin. These formulations are designed for localized treatment of superficial fungal infections like athlete’s foot, ringworm, and yeast infections.
- Oral Medications: In some cases, miconazole is administered orally to treat systemic fungal infections. This route is typically reserved for more severe or disseminated infections.
- Vaginal Suppositories: Miconazole is also available in vaginal suppository form to treat vaginal yeast infections. These are designed for localized action within the vagina.
Dosage and Administration
The appropriate dosage and administration of miconazole depend heavily on the specific formulation and the nature of the infection. Always adhere to the instructions provided by your healthcare provider. The dosage and frequency of application can vary considerably. Incorrect usage can lead to treatment failure or adverse effects.
Comparison of Miconazole Formulations
The following table provides a comparative overview of various miconazole strengths and formulations. Note that specific dosages and indications may vary based on the product and prescribing guidelines.
| Formulation | Strength (mg/g or %) | Typical Indication | Notes |
|---|---|---|---|
| Cream | 2% | Superficial skin infections | Apply thinly to affected area, as directed |
| Cream | 1% | Superficial skin infections | Apply thinly to affected area, as directed |
| Ointment | 2% | Superficial skin infections | Apply thinly to affected area, as directed |
| Vaginal Suppositories | 100mg | Vaginal yeast infections | Insert suppository as directed, usually once daily |
| Oral Tablets | 100mg | Systemic fungal infections | Follow dosage instructions carefully |
Comparing Tioconazole and Miconazole: Tioconazole Vs Miconazole What Are The Differences
Tioconazole and miconazole are both imidazole antifungals commonly used to treat various superficial fungal infections. Understanding their similarities and differences is crucial for selecting the appropriate medication for a specific patient. This comparison delves into their mechanisms of action, pharmacokinetics, efficacy, and safety profiles to aid in informed decision-making.
Mechanisms of Action Comparison
Tioconazole and miconazole both inhibit fungal cell membrane synthesis. They achieve this by disrupting the ergosterol synthesis pathway in fungal cells. Ergosterol is a crucial component of the fungal cell membrane, and its disruption leads to membrane damage and ultimately, fungal death. However, the specific mechanisms through which they achieve this disruption differ slightly. Tioconazole is thought to act primarily by inhibiting the enzyme lanosterol 14α-demethylase, an essential enzyme in ergosterol biosynthesis.
Miconazole, on the other hand, interferes with the conversion of lanosterol to ergosterol at multiple steps in the pathway.
Pharmacokinetic Differences, Tioconazole vs miconazole what are the differences
Absorption, distribution, metabolism, and excretion (ADME) profiles significantly influence the efficacy and safety of these drugs. Tioconazole is known for its good absorption from the skin, and miconazole also exhibits reasonable skin absorption. However, their systemic bioavailability varies. Tioconazole is more likely to be absorbed systemically compared to miconazole, potentially leading to different side effect profiles. Distribution patterns in the body also vary, affecting the extent to which the drug reaches the site of infection.
Metabolism and excretion routes further contribute to the overall pharmacokinetic profile of each drug.
Efficacy and Safety Comparison
The efficacy and safety profiles of tioconazole and miconazole in treating specific fungal infections are summarized in the following table.
| Characteristic | Tioconazole | Miconazole |
|---|---|---|
| Efficacy (in treating superficial mycoses) | Generally effective against dermatophytes, yeasts, and some molds. | Generally effective against dermatophytes, yeasts, and some molds. |
| Safety Profile (Adverse effects) | Generally well-tolerated, but some patients may experience local skin reactions like irritation or burning. Rare cases of systemic effects have been reported. | Generally well-tolerated, but local skin reactions such as itching and burning are possible. Systemic effects are less common but possible. |
| Specific fungal infections | Effective against tinea corporis, tinea cruris, and tinea pedis. | Effective against tinea corporis, tinea cruris, and tinea pedis. |
| Susceptibility patterns | Variations exist in susceptibility depending on the fungal species. Clinicians should consider local resistance patterns. | Variations exist in susceptibility depending on the fungal species. Clinicians should consider local resistance patterns. |
Spectrum of Activity
The spectrum of activity against different fungal species is an important consideration in choosing between tioconazole and miconazole. While both are effective against a broad range of dermatophytes and yeasts, some species may show varying degrees of susceptibility. Tioconazole, for example, may have slightly improved activity against certain yeasts, while miconazole may be slightly more effective against specific dermatophytes.
Clinical guidelines often recommend considering the specific fungal species involved in the infection before choosing between the two medications. In cases of suspected resistance, additional diagnostic testing or alternative treatment options should be considered.
Indications and Usage

Tioconazole and miconazole are both imidazole antifungals commonly prescribed for superficial fungal infections. Understanding their specific applications and relative strengths is crucial for appropriate treatment. This section details the common types of fungal infections where each drug excels, providing a comparative analysis to guide informed decisions.
Ever wondered about the differences between tioconazole and miconazole for fungal infections? While those topical treatments are important, it’s crucial to remember a healthy lifestyle is key, including watching your diet. For example, limiting high-sodium foods and processed snacks, as well as those high in saturated fats can be essential for controlling blood pressure. Checking out worst foods for high blood pressure can offer valuable insights.
Ultimately, consulting a doctor about the best treatment for your specific fungal infection remains important, alongside dietary considerations.
Tioconazole Indications
Tioconazole is primarily indicated for treating superficial dermatophyte infections, such as athlete’s foot, ringworm (tinea corporis), and jock itch (tinea cruris). It effectively targets the dermatophytes that cause these infections. It is also used in the treatment of yeast infections, particularly those affecting the skin folds (such as the groin or armpits) and in some cases, onychomycosis (nail fungus).
These infections are characterized by skin lesions, itching, and scaling.
Miconazole Indications
Miconazole is a broad-spectrum antifungal, showing effectiveness against various types of superficial fungal infections. It’s frequently prescribed for candidiasis (yeast infections) of the skin, mouth, vagina, and nails. It’s also used in the treatment of dermatophytoses, similar to tioconazole, including athlete’s foot, ringworm, and jock itch. Its efficacy extends to certain types of pityriasis versicolor, a superficial fungal infection that causes skin discoloration.
Comparative Table of Indications
| Drug | Fungal Infection | Body Site | Patient Population | Strengths |
|---|---|---|---|---|
| Tioconazole | Dermatophytes (athlete’s foot, ringworm, jock itch), Yeast infections (skin folds), Onychomycosis (in some cases) | Skin, nails, groin, armpits | Adults and children with superficial fungal infections | Effective against dermatophytes and yeast infections in affected areas. Potentially less expensive than some other options. |
| Miconazole | Dermatophytes (athlete’s foot, ringworm, jock itch), Candidiasis (skin, mouth, vagina, nails), Pityriasis versicolor (in some cases) | Skin, nails, mouth, vagina, groin, armpits | Adults and children with various superficial fungal infections, including those with candidiasis | Broader spectrum of activity, effective against various types of fungi and infections in different body areas. Available in numerous formulations. |
Relative Strengths for Specific Infections
While both tioconazole and miconazole effectively treat many fungal infections, their relative strengths vary depending on the specific type of infection. For example, tioconazole might be a slightly more targeted approach for dermatophyte infections, while miconazole might be preferred in situations involving candidiasis due to its broader spectrum of activity. A healthcare provider will consider the specific type of infection, its location, and the patient’s overall health when determining the most appropriate treatment.
Patient response to the medication should also be monitored closely, and adjustments may be necessary.
Potential Side Effects

Both tioconazole and miconazole, while effective antifungal medications, can cause various side effects. Understanding these potential reactions is crucial for responsible use and proactive management. Knowing the potential side effects can help patients and healthcare providers make informed decisions about treatment options.
Tioconazole Side Effects
Tioconazole, a topical antifungal, is generally well-tolerated. However, some individuals may experience localized reactions at the application site. These reactions often include skin irritation, redness, burning, itching, and stinging. Less frequently, systemic reactions like allergic reactions or contact dermatitis might occur. In rare instances, more severe reactions like skin rashes or swelling could develop.
Miconazole Side Effects
Miconazole, also a topical antifungal, shares some common side effects with tioconazole, primarily localized reactions. Skin irritation, redness, burning, and itching are common. These reactions typically occur at the application site and are usually mild to moderate. While allergic reactions are less frequent than with some other medications, they can manifest as hives or swelling. Rarely, more serious reactions such as severe skin rashes or difficulty breathing might be observed.
Comparison of Side Effects
| Adverse Reaction | Tioconazole (Frequency/Severity) | Miconazole (Frequency/Severity) |
|---|---|---|
| Skin Irritation | Common, usually mild to moderate | Common, usually mild to moderate |
| Redness | Common, usually mild to moderate | Common, usually mild to moderate |
| Burning Sensation | Common, usually mild to moderate | Common, usually mild to moderate |
| Itching | Common, usually mild to moderate | Common, usually mild to moderate |
| Stinging | Common, usually mild to moderate | Common, usually mild to moderate |
| Allergic Reactions | Less frequent, but can be severe | Less frequent, but can be severe |
| Contact Dermatitis | Rare | Rare |
| Severe Skin Rashes | Rare | Rare |
| Systemic Reactions | Rare | Rare |
Managing and Avoiding Side Effects
Applying a thin layer of the medication, as directed by a healthcare professional, can help minimize localized reactions. Using a barrier cream or ointment over the affected area might alleviate irritation. If symptoms worsen or persist, it’s essential to seek medical advice. Reporting any unusual reactions to the healthcare provider is crucial for appropriate management. Patients should also be aware of potential interactions with other medications they might be taking.
Adherence to the prescribed dosage and application instructions can help to reduce the likelihood of side effects.
Drug Interactions
Understanding potential drug interactions is crucial when using antifungal medications like tioconazole and miconazole. These interactions can significantly affect the efficacy of the treatment or increase the risk of adverse effects. Careful consideration of concurrent medications is essential for safe and effective therapy.Interactions between antifungal medications and other drugs can occur through various mechanisms. These include competition for metabolic pathways, alteration of drug absorption or elimination, and potentiation or inhibition of the effects of one or more drugs.
It’s important to recognize these potential interactions to avoid adverse consequences and ensure optimal patient outcomes.
Potential Tioconazole Interactions
Tioconazole, a topical antifungal, can interact with certain medications. These interactions are often related to its potential to affect liver function or other organ systems. It’s essential to carefully review the patient’s medication history to identify potential interactions.
- Certain medications that affect liver enzymes, such as some antibiotics or anti-inflammatory drugs, may potentially increase the risk of liver toxicity if used concurrently with tioconazole. Monitoring liver function tests is vital when combining tioconazole with these agents.
- Drugs that are metabolized by the same enzymes as tioconazole may impact its clearance. This can lead to either increased or decreased tioconazole levels in the body, potentially affecting its effectiveness or causing adverse effects.
- Tioconazole, like other topical medications, can be absorbed into the bloodstream, although to a lesser extent. The potential for interactions with systemic medications should not be disregarded, even if the drug is intended for topical use.
Potential Miconazole Interactions
Miconazole, another topical antifungal, also has the potential for drug interactions, particularly when used systemically. Many of these interactions relate to its effects on the liver and kidneys. Always check the prescribing information for miconazole for a complete list of potential interactions.
- Miconazole can interact with medications that affect liver function or renal elimination. This is particularly important when using miconazole orally or intravenously, as these formulations have a greater potential for systemic absorption and interaction with other medications.
- Miconazole may affect the metabolism of other drugs, either increasing or decreasing their levels in the blood. This can impact the effectiveness or safety of the co-administered medication.
- Some medications may interfere with the absorption or excretion of miconazole. This may alter the therapeutic effectiveness or increase the risk of adverse effects. Monitoring for any changes in the drug’s effectiveness or the emergence of unusual side effects is crucial when co-administering medications.
Table of Potential Drug Interactions
| Medication Class | Potential Interaction with Tioconazole | Potential Interaction with Miconazole | Notes |
|---|---|---|---|
| Hepatic Enzyme Inhibitors | Increased risk of liver toxicity | Increased risk of liver toxicity | Careful monitoring of liver function tests is essential. |
| CYP3A4 Inhibitors | Potential for increased tioconazole levels and adverse effects | Potential for increased miconazole levels and adverse effects | Consult prescribing information. |
| Renal Elimination Drugs | Potential for increased tioconazole levels and adverse effects (if renal impairment exists) | Potential for increased miconazole levels and adverse effects (if renal impairment exists) | Assess renal function before co-administration. |
| Oral Contraceptives | Potential for decreased contraceptive efficacy (in some cases) | Potential for decreased contraceptive efficacy (in some cases) | Advise patients on alternative birth control methods. |
Interactions of Particular Concern
Several interactions warrant particular attention. These include those that involve medications known to affect the liver or kidneys. Patients with pre-existing liver or kidney disease are at higher risk of adverse effects. Always consult with a healthcare professional before combining tioconazole or miconazole with other medications.
Special Considerations
Choosing between tioconazole and miconazole depends on various factors, including the specific condition, patient characteristics, and potential risks. Understanding the unique considerations for different patient populations is crucial for safe and effective treatment. Special attention must be paid to potential interactions and side effects, particularly in vulnerable groups like pregnant women and children.
Special Considerations for Pregnant Women
Pregnancy presents unique challenges for antifungal therapy. Both tioconazole and miconazole have demonstrated potential for placental transfer and are not without potential risks to the developing fetus. Therefore, careful consideration of the benefits and risks is necessary. For example, a pregnant woman with a severe vaginal yeast infection might require treatment, but the choice of medication should be guided by the potential for fetal harm and the severity of the infection.
Special Considerations for Children
Dosage adjustments and potential side effects are key considerations for using these medications in children. The developing organs and immune systems of children can react differently to medication compared to adults. Furthermore, the optimal treatment approach for pediatric patients often necessitates a more nuanced consideration of the infection’s severity and the child’s overall health. For instance, a child with a mild skin infection might not require systemic antifungal treatment, while a more severe case might benefit from topical application.
Special Considerations for Patients with Renal Impairment
Renal impairment can affect how the body processes and eliminates medications. Both tioconazole and miconazole can be excreted through the kidneys. If a patient has impaired kidney function, dosage adjustments may be necessary to prevent potentially toxic buildup in the body. This is critical to consider to avoid adverse reactions. For example, a patient with chronic kidney disease requiring antifungal therapy should have their renal function evaluated before starting either medication and should be monitored closely during treatment.
Special Considerations for Patients with Liver Impairment
Liver impairment can also influence the metabolism and excretion of tioconazole and miconazole. Both drugs undergo significant hepatic metabolism. Therefore, in patients with liver disease, a lower dosage or a different administration schedule might be necessary to prevent potential toxicity. For instance, a patient with cirrhosis of the liver would require careful monitoring of liver function tests and potential dosage adjustments when prescribed either medication.
Table of Special Considerations
| Patient Population | Contraindications | Precautions |
|---|---|---|
| Pregnant Women | Limited data, potential for placental transfer, fetal harm should be considered. | Use lowest effective dose, monitor for fetal effects. |
| Children | Limited data on long-term effects, potential for adverse reactions. | Dosage adjustments based on weight and age, use topical preparations when appropriate. |
| Renal Impairment | May lead to drug accumulation, potentially toxic effects. | Dosage adjustments, monitoring of renal function. |
| Liver Impairment | May lead to drug accumulation, potentially toxic effects. | Dosage adjustments, monitoring of liver function. |
Differences in Recommendations for Different Age Groups
The recommended dosage and administration routes of tioconazole and miconazole often differ significantly between adults and children. For instance, while adults may receive oral medications, topical formulations might be preferred in children due to the potential for adverse systemic effects. Moreover, careful consideration must be given to the specific type of fungal infection and the patient’s overall health status.
Final Summary
In conclusion, while both tioconazole and miconazole are effective antifungal agents, their specific applications and potential side effects differ. Understanding these distinctions allows for a more informed approach to treating fungal infections. Consulting with a healthcare professional is essential for determining the most appropriate treatment plan for individual needs. Remember, this information is for educational purposes only and should not be considered medical advice.