Maitake Mushroom Benefits Nutrition & More
Maitake mushroom benefits nutrition is a fascinating subject, delving into the incredible nutritional profile and potential health advantages of this...







Maitake mushroom benefits nutrition is a fascinating subject, delving into the incredible nutritional profile and potential health advantages of this...
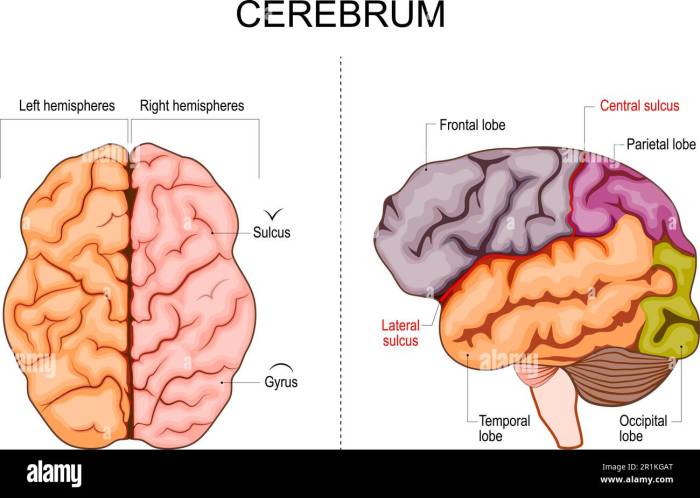
Dysesthesia and multiple sclerosis: a complex interplay of nerve damage and sensory disturbance. This exploration delves into the various forms...
Does this stabbing headache mean I have MS? This question haunts many, and this post delves deep into the complexities...
Do I have PMS? This exploration delves into the fascinating world of premenstrual syndrome, unraveling its symptoms, triggers, and management...
Lovenox enoxaparin vs heparin: Understanding the nuances of these anticoagulants is crucial for effective blood clot prevention. Each medication plays...
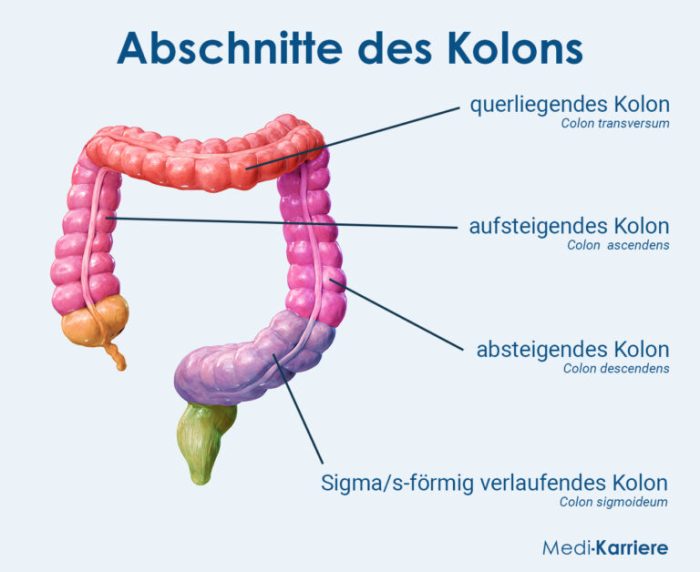
Prune juice for constipation is a popular remedy for those struggling with this common digestive issue. This comprehensive guide explores...
Heart failure medications types and available options offer a crucial path to managing this complex condition. Understanding the various types...
Aloe vera for hair growth is a popular topic, but how much truth is behind the hype? This post explores...
Cholesterol drug helps remove pfas study reveals a potential new avenue for tackling PFAS contamination. This groundbreaking research explores the...
Facts about tension headaches: These common headaches, often described as a tight band around the head, affect millions worldwide. This...