Paroxysmal nocturnal dyspnea pnd – Paroxysmal nocturnal dyspnea (PND) is a sudden, overwhelming shortness of breath that typically awakens a person from sleep. This condition, often triggered by underlying heart or lung problems, can be incredibly disruptive to daily life. We’ll delve into the causes, symptoms, diagnosis, treatment, and potential complications of PND, offering a comprehensive understanding of this challenging respiratory condition.
PND is characterized by a rapid onset of shortness of breath, usually occurring during the night or early morning hours. This often leads to a person sitting up or standing to alleviate the discomfort. Understanding the triggers and contributing factors is crucial for effective management.
Defining Paroxysmal Nocturnal Dyspnea (PND)
Paroxysmal nocturnal dyspnea (PND) is a sudden and severe shortness of breath that awakens a person from sleep. This condition is often a symptom of an underlying heart problem, typically involving fluid buildup in the lungs. Understanding its triggers and symptoms is crucial for effective diagnosis and management.The pathophysiology of PND revolves around the heart’s inability to adequately pump blood, leading to fluid accumulation in the lungs.
As a person lies down at night, the fluid in the body shifts, increasing pressure in the pulmonary capillaries. This increased pressure causes fluid to leak into the alveoli, the tiny air sacs in the lungs, making it difficult to breathe. This buildup of fluid in the lungs is a key factor in the sudden onset of shortness of breath.
Key Characteristics of PND
PND is characterized by sudden, severe shortness of breath that typically occurs at night, often after a few hours of sleep. It’s a common symptom of heart failure, with a strong correlation between the severity of heart failure and the frequency and intensity of PND episodes. The symptoms usually begin gradually, with increasing difficulty breathing, and may even be accompanied by a feeling of suffocation.
Symptoms Associated with PND
The symptoms of PND typically include:
- Sudden onset of shortness of breath, often during sleep.
- Feeling of tightness or pressure in the chest.
- Coughing, sometimes with frothy or blood-tinged sputum.
- Rapid heart rate (tachycardia).
- Anxiety and restlessness.
- A sense of suffocation or drowning.
These symptoms usually worsen when lying down and improve when sitting or standing upright. This positional change facilitates the drainage of fluid from the lungs, alleviating the breathing difficulty. The rapid onset of symptoms and their typical progression are characteristic of PND.
Paroxysmal nocturnal dyspnea (PND) is a sudden, intense shortness of breath that typically wakes you up at night. It’s often a symptom of a more serious heart condition, and sometimes a double bypass heart surgery what is a double bypass heart surgery might be needed to improve blood flow and alleviate the symptoms. Understanding the underlying causes and treatment options for PND is crucial for managing this frustrating condition.
Comparison with Other Respiratory Conditions
| Feature | Paroxysmal Nocturnal Dyspnea (PND) | Asthma | Chronic Obstructive Pulmonary Disease (COPD) ||—|—|—|—|| Onset | Sudden, typically at night | Gradual, can occur throughout the day | Gradual, often progressive, throughout the day || Positional effect | Worsens when lying down, improves when sitting up | Less pronounced positional effect, but symptoms can worsen with exertion | Less pronounced positional effect || Underlying cause | Usually heart failure | Airways inflammation and narrowing | Lung damage and airway obstruction || Symptoms | Sudden shortness of breath, coughing, chest tightness | Wheezing, coughing, chest tightness | Chronic cough, shortness of breath, mucus production |This table highlights the key differences in symptom onset, positionality, and underlying causes between PND and other common respiratory conditions.
Accurate diagnosis relies on a careful evaluation of these distinctions, along with a comprehensive medical history. A patient experiencing symptoms suggestive of PND should seek prompt medical attention for proper diagnosis and treatment.
Identifying Risk Factors for PND
Paroxysmal nocturnal dyspnea (PND) is a distressing symptom often linked to underlying heart conditions. Understanding the factors that increase susceptibility to PND is crucial for early diagnosis and effective management. Identifying these risk factors allows healthcare professionals to proactively assess patients at higher risk and implement preventative measures.Recognizing the predisposing conditions and their influence on PND development empowers individuals to make informed lifestyle choices and engage in proactive health management.
This knowledge also allows for targeted interventions and personalized treatment strategies.
Predisposing Medical Conditions
Several medical conditions significantly increase the risk of developing PND. These conditions often involve impaired heart function or fluid retention. Conditions like congestive heart failure (CHF) are a primary driver. The strain on the heart during sleep can lead to fluid buildup in the lungs, causing the characteristic shortness of breath. Other conditions that may contribute include coronary artery disease, pulmonary hypertension, and valvular heart disease.
These conditions impede the heart’s ability to effectively pump blood, potentially triggering fluid overload and the resultant PND symptoms.
Role of Lifestyle Factors
Lifestyle choices can significantly impact the risk of developing PND. Obesity, a prevalent health concern, is linked to an increased risk due to the added strain on the cardiovascular system. Smoking and a sedentary lifestyle further contribute to this increased risk. Excessive alcohol consumption can also exacerbate fluid retention and increase the likelihood of developing PND. Poorly managed stress and lack of adequate sleep can also play a role.
Paroxysmal nocturnal dyspnea (PND) is a sudden, severe shortness of breath that usually happens at night. It’s often a symptom of a more serious underlying heart condition, but sometimes it can be linked to other issues. Understanding the complexities of PND requires looking at other related medical conditions. For example, it’s important to differentiate PND from language disorders like Broca’s aphasia, which affects the ability to produce speech.
Learning about what is Broca’s aphasia can help you appreciate the nuanced differences between respiratory and neurological issues. Ultimately, accurately diagnosing PND requires a comprehensive approach that considers a wide range of potential causes.
A comprehensive approach to health management, including diet, exercise, and stress reduction, is vital in mitigating these risks.
Paroxysmal nocturnal dyspnea (PND) can be a really scary experience, waking you up gasping for air. It’s often a symptom of an underlying heart condition, but sometimes it can be linked to other things. For example, if you’re wondering if you might have premenstrual syndrome (PMS), checking out this resource on do i have pms could help you understand potential causes and treatment options.
Ultimately, though, if you’re experiencing PND, it’s crucial to see a doctor to get a proper diagnosis and treatment plan.
Demographic Variations in Risk
The risk of developing PND varies across different demographics. Older adults are at a higher risk, as age-related cardiovascular changes can increase the likelihood of developing conditions such as CHF. Men and women experience different patterns of cardiovascular disease progression. While heart disease is often associated with men in some studies, women may experience different risk factors and present with distinct symptoms.
This highlights the need for personalized approaches to risk assessment and management, taking into account age and gender-specific factors.
Summary Table of Risk Factors
| Risk Factor | Severity | Potential Impact |
|---|---|---|
| Congestive Heart Failure (CHF) | High | Significant strain on the heart, leading to fluid buildup and shortness of breath, particularly at night. |
| Coronary Artery Disease (CAD) | Moderate to High | Reduced blood flow to the heart, potentially leading to heart failure and PND. |
| Pulmonary Hypertension | High | Increased pressure in the blood vessels of the lungs, hindering blood flow and increasing the risk of fluid buildup in the lungs. |
| Obesity | Moderate | Increased strain on the heart, leading to potential heart failure and PND. |
| Smoking | High | Damages blood vessels, increasing the risk of heart disease and PND. |
| Sedentary Lifestyle | Moderate | Contributes to weight gain and increases the risk of heart disease, potentially leading to PND. |
| Age (older adults) | Moderate to High | Age-related cardiovascular changes can increase the risk of conditions like CHF, leading to PND. |
Symptoms and Diagnosis of PND
Paroxysmal nocturnal dyspnea (PND) is a distressing condition characterized by sudden episodes of shortness of breath that typically occur at night. Understanding the specific symptoms and diagnostic procedures is crucial for timely intervention and effective management. This understanding empowers both patients and healthcare providers to identify the underlying cause and implement appropriate treatment strategies.Recognizing the hallmark symptoms of PND is paramount for prompt diagnosis.
These symptoms often present in a specific pattern, allowing healthcare professionals to differentiate PND from other respiratory conditions. The distinctive nature of the symptoms, combined with a thorough patient history, facilitates accurate diagnosis and treatment planning.
Typical Symptoms of PND
The hallmark symptom of PND is sudden, severe shortness of breath, typically occurring at night or in the early morning hours. This symptom is often accompanied by other indicators, distinguishing it from other respiratory issues. Patients may describe the sensation as an urgent need to sit up or stand to alleviate the breathlessness.These symptoms frequently include:
- Sudden onset of shortness of breath, typically at night or in the early morning hours.
- A feeling of tightness or pressure in the chest.
- A rapid heart rate (tachycardia).
- Coughing, often with frothy or blood-tinged sputum.
- Cold sweats.
- Anxiety or a sense of impending doom.
Diagnostic Procedures for PND
A comprehensive approach to diagnosing PND involves a multifaceted evaluation. The diagnostic process begins with a detailed patient history to understand the specific symptoms, their duration, and any associated factors.The diagnostic procedures include:
- Thorough Patient History: A detailed patient history, including the frequency, timing, and precipitating factors of the shortness of breath, is essential. Factors like recent illnesses, medications, and lifestyle habits provide crucial insights.
- Physical Examination: A physical examination focuses on assessing vital signs, including respiratory rate, heart rate, and blood pressure. Auscultation of the lungs and heart is performed to detect any abnormalities suggestive of heart failure or other underlying conditions.
- Diagnostic Tests: These tests can help determine the underlying cause of PND. Common tests include:
- Chest X-ray: A chest X-ray can reveal evidence of pulmonary edema or other abnormalities.
- Electrocardiogram (ECG): An ECG helps evaluate heart rhythm and detect any underlying cardiac conditions.
- Echocardiogram: This test provides detailed information about the structure and function of the heart, identifying potential heart valve abnormalities or other structural issues.
- Blood tests: Blood tests, such as BNP (brain natriuretic peptide) levels, can indicate the presence of heart failure.
- Further Investigations: In some cases, further investigations, such as sleep studies, may be necessary to rule out other sleep-related breathing disorders.
Differential Diagnoses for PND
Accurate diagnosis necessitates differentiating PND from other conditions that can mimic its symptoms. The following table Artikels key differential diagnoses, highlighting the distinguishing features.
| Differential Diagnosis | Distinguishing Features |
|---|---|
| Asthma | Symptoms often worsen at night, but the onset is usually gradual. Wheezing and chest tightness are common. |
| Chronic Obstructive Pulmonary Disease (COPD) | Progressive shortness of breath, often associated with a history of smoking. Cough and sputum production are common. |
| Congestive Heart Failure (CHF) | Symptoms often worsen with exertion and at night. Other symptoms, such as edema, may also be present. |
| Pulmonary Embolism | Sudden onset of shortness of breath, often accompanied by chest pain and other symptoms. A history of recent travel or surgery may be present. |
| Anxiety Disorder | Shortness of breath can occur, but often accompanied by other anxiety symptoms, such as palpitations and fear. |
Treatment and Management of PND
Paroxysmal nocturnal dyspnea (PND) is a distressing condition that requires a multifaceted approach to management. Effective treatment addresses both the acute episodes of shortness of breath and the underlying heart or lung conditions that cause them. Understanding the specific triggers and contributing factors is crucial for developing a personalized treatment plan.
Acute Management Strategies
Effective acute management of PND focuses on rapidly alleviating symptoms and restoring comfort. This often involves a combination of interventions aimed at improving breathing and reducing fluid buildup. Oxygen therapy, elevating the head of the bed, and using medications to reduce fluid retention are common strategies.
- Oxygen Therapy: Supplemental oxygen can help improve oxygen levels in the blood, reducing the sensation of breathlessness. This is often administered through nasal cannulas or masks, and the dosage is adjusted based on individual needs and blood oxygen saturation levels.
- Positioning: Elevating the head of the bed significantly reduces fluid buildup in the lungs. Raising the head of the bed by 6-8 inches can make a notable difference. This is crucial in relieving the pressure on the lungs and facilitating easier breathing.
- Medications: Medications such as diuretics, which promote fluid excretion, and vasodilators, which widen blood vessels, are often used to address the underlying causes and manage acute symptoms. These medications help reduce fluid buildup in the lungs, improving breathing and overall comfort. Examples of these medications include furosemide (Lasix) and nitroglycerin.
Chronic Management Strategies
Chronic management of PND aims at preventing future episodes and improving overall health. This often involves addressing the underlying conditions that cause the episodes.
- Heart Failure Management: For patients with heart failure, managing the condition with medications, lifestyle changes, and regular follow-up appointments with their cardiologist is crucial. This may include medications like ACE inhibitors, beta-blockers, and digoxin, which are used to improve heart function and reduce fluid buildup.
- Lung Disease Management: If PND is related to lung disease, treating the underlying condition is vital. This might involve medications for asthma or chronic obstructive pulmonary disease (COPD), pulmonary rehabilitation, and other treatments as recommended by a pulmonologist.
Lifestyle Modifications
Lifestyle changes play a significant role in managing PND. Dietary adjustments, weight management, and regular exercise can all contribute to improved overall health and reduce the frequency and severity of PND episodes.
- Dietary Changes: A low-sodium diet is often recommended to minimize fluid retention. Reducing fluid intake before bed can also be helpful.
- Weight Management: Maintaining a healthy weight is important for overall cardiovascular health and can reduce strain on the heart, thus minimizing PND episodes.
- Regular Exercise: Regular exercise, tailored to individual capabilities, can improve cardiovascular function and reduce the risk of heart failure, a major contributor to PND. It’s essential to consult a doctor before starting any new exercise regimen.
Medication Table
| Medication | Mechanism of Action | Potential Side Effects |
|---|---|---|
| Furosemide (Lasix) | Diuretic, increases urine output | Dehydration, electrolyte imbalances, dizziness, nausea |
| Digoxin | Strengthens heart contractions | Nausea, vomiting, diarrhea, visual disturbances |
| ACE Inhibitors | Relax blood vessels, reduce strain on the heart | Cough, dizziness, fatigue, kidney problems |
| Nitroglycerin | Vasodilator, widens blood vessels | Headache, dizziness, lightheadedness |
Complications Associated with PND: Paroxysmal Nocturnal Dyspnea Pnd
Paroxysmal nocturnal dyspnea (PND) is a distressing symptom often indicating an underlying heart condition. While treatment focuses on managing the acute episodes, it’s crucial to understand the potential complications that can arise from untreated or poorly managed PND. These complications can significantly impact a patient’s quality of life and overall health.Untreated or poorly managed PND can lead to a cascade of adverse effects, extending beyond the initial discomfort.
The severity of these complications varies depending on the underlying cause and the promptness of treatment. Recognizing these potential issues is vital for proactive management and improved patient outcomes.
Potential Cardiovascular Complications
Cardiovascular issues are a primary concern in PND. The repeated episodes of shortness of breath can strain the heart, potentially leading to various complications. Left ventricular dysfunction, a weakening of the heart’s ability to pump blood efficiently, is a serious concern. This can progress to heart failure, a condition characterized by the heart’s inability to meet the body’s needs.
Further, pulmonary hypertension, elevated blood pressure in the blood vessels leading to the lungs, is another potential complication. This condition can worsen PND and eventually lead to respiratory failure.
Respiratory Complications
The persistent shortness of breath associated with PND can lead to respiratory complications. Repeated episodes can damage the lungs, leading to chronic lung diseases. Individuals with PND may experience a decrease in lung function over time, affecting their ability to breathe adequately. This can lead to a reduced quality of life and increased reliance on supplemental oxygen.
Other Potential Complications
PND can also lead to complications in other body systems. For example, the constant strain on the body from PND episodes can lead to fatigue and reduced physical activity. This can contribute to a decrease in overall well-being and make daily tasks challenging. Furthermore, PND can also contribute to anxiety and depression due to the persistent fear of future episodes and the impact on daily life.
Impact on Quality of Life
The complications of PND significantly impact a patient’s quality of life. Chronic fatigue, reduced physical activity, and the fear of future episodes can lead to social isolation and decreased participation in activities. The emotional toll of living with PND can be substantial, impacting mental health and overall well-being. The need for ongoing medical care and monitoring can also create additional stress and inconvenience for patients and their families.
Summary of Complications
| Complication | Frequency | Severity |
|---|---|---|
| Left ventricular dysfunction | High | High |
| Heart failure | High | High |
| Pulmonary hypertension | Moderate | Moderate to High |
| Chronic lung diseases | Moderate | Moderate |
| Fatigue and reduced physical activity | High | Moderate |
| Anxiety and depression | Variable | Moderate to High |
Note: Frequency and severity are relative and can vary based on individual factors and management strategies. Consulting with a healthcare professional is essential for accurate assessment and personalized management plans.
Prevention Strategies for PND
Paroxysmal nocturnal dyspnea (PND) is a distressing symptom, often signaling underlying heart conditions. While a cure for PND hinges on addressing the root cause, proactive measures can significantly reduce the frequency and severity of episodes. These preventive strategies focus on lifestyle modifications, early detection of potential triggers, and consistent medical management. A holistic approach to PND prevention empowers individuals to live more comfortably and avoid exacerbations.Effective prevention of PND involves a multifaceted approach, encompassing lifestyle changes, vigilant monitoring of underlying conditions, and proactive medical interventions.
This comprehensive strategy is crucial in mitigating the impact of PND and improving overall well-being.
Lifestyle Modifications for Preventing PND
Lifestyle choices play a critical role in managing PND. Modifying certain habits can reduce the strain on the cardiovascular system and lessen the likelihood of PND episodes. Consistent adherence to these modifications is key to long-term success.
- Maintaining a Healthy Weight: Excess weight puts extra pressure on the heart, increasing the risk of heart failure and subsequent PND episodes. Achieving and maintaining a healthy weight through a balanced diet and regular exercise can significantly reduce the risk of PND.
- Regular Exercise: Physical activity strengthens the heart and improves overall cardiovascular health. Regular exercise, ideally at least 30 minutes most days of the week, promotes better blood circulation and reduces the strain on the heart.
- Dietary Adjustments: A diet rich in fruits, vegetables, and whole grains, and low in saturated and trans fats, cholesterol, and sodium can help maintain a healthy weight and cardiovascular function, indirectly reducing the risk of PND.
- Stress Management Techniques: Chronic stress can exacerbate existing heart conditions and trigger PND episodes. Incorporating stress-reducing techniques such as yoga, meditation, or deep breathing exercises can help regulate stress levels and minimize the risk of PND.
Early Detection and Treatment of Underlying Conditions
Prompt diagnosis and management of underlying heart conditions are essential in preventing PND. Regular check-ups with a cardiologist, along with adhering to prescribed medications, are crucial preventative measures.
- Regular Check-ups: Regular appointments with a cardiologist allow for early detection of potential issues, enabling timely interventions and preventing progression to more severe conditions that might lead to PND.
- Adherence to Medications: Strict adherence to prescribed medications, including diuretics, ACE inhibitors, or beta-blockers, as recommended by the physician, helps maintain stable blood pressure and fluid balance, reducing the risk of PND.
- Management of Co-morbidities: Conditions like hypertension, diabetes, and sleep apnea often contribute to heart conditions. Addressing these co-morbidities through appropriate treatment can significantly lower the risk of PND.
Preventative Actions and Their Benefits
Implementing preventative strategies offers significant advantages in reducing the likelihood of PND. A proactive approach can substantially improve quality of life and reduce the need for emergency interventions.
- Maintaining a healthy weight: Reduces strain on the heart, lowering the risk of heart failure and PND episodes. Example: A patient with a history of PND who loses weight and maintains a healthy BMI experiences a significant reduction in PND episodes.
- Regular exercise: Strengthens the heart, improves circulation, and reduces strain on the cardiovascular system. Example: A patient who incorporates regular exercise into their routine observes fewer episodes of PND compared to a patient who does not.
- Dietary adjustments: A balanced diet lowers the risk of cardiovascular disease, reducing the risk of PND. Example: A patient adopting a heart-healthy diet with low sodium intake experiences fewer instances of PND compared to a patient who consumes a diet high in saturated fats.
- Stress management techniques: Reduces stress levels, preventing exacerbations of underlying heart conditions and PND episodes. Example: A patient with chronic stress who implements stress management techniques notices fewer episodes of PND.
- Regular check-ups: Early detection and treatment of underlying conditions prevents progression to severe heart conditions. Example: A patient who follows a routine of regular check-ups and medication adherence experiences a notable reduction in PND episodes and avoids potentially life-threatening complications.
Case Studies and Illustrations
Paroxysmal nocturnal dyspnea (PND) is a distressing condition characterized by sudden episodes of shortness of breath, typically occurring at night. Understanding the diagnostic process, treatment approaches, and impact on patients’ lives is crucial for effective management. This section delves into case studies, illustrations, and personal accounts to provide a more comprehensive understanding of PND.
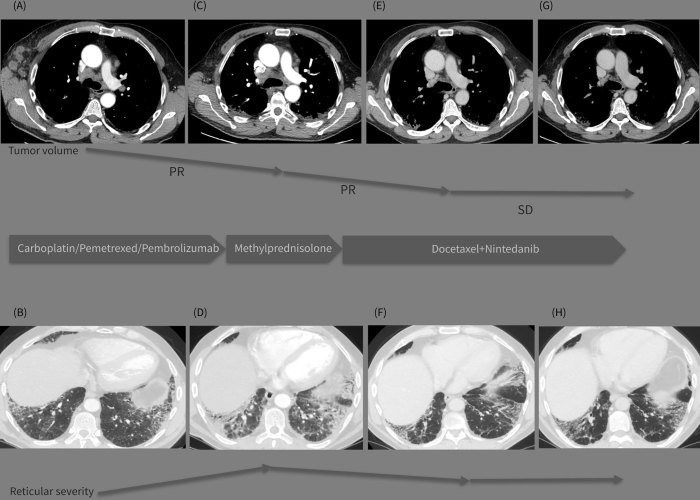
A Case Study of a Patient with PND
A 65-year-old male patient presented with recurrent episodes of severe shortness of breath, particularly at night. The symptoms typically began a few hours after lying down and were accompanied by coughing and wheezing. Initial assessments revealed a history of hypertension and coronary artery disease. Physical examination showed elevated blood pressure and diminished breath sounds in the lower lung fields.
The patient’s electrocardiogram (ECG) revealed signs of left ventricular hypertrophy. Further diagnostic testing, including a chest X-ray and echocardiogram, confirmed the presence of pulmonary edema and an enlarged heart. The diagnosis of congestive heart failure, a common cause of PND, was established. Treatment involved diuretics to reduce fluid retention, beta-blockers to control heart rate, and medications to manage hypertension.
Regular follow-up visits and lifestyle modifications, including dietary changes and exercise, were also implemented. The patient’s symptoms significantly improved with the prescribed treatment regimen, allowing him to maintain a satisfactory quality of life.
Illustrative Depiction of Anatomical Structures and Physiological Processes
The physiological processes underlying PND are primarily related to fluid buildup in the lungs. Congestive heart failure, a common cause, leads to inadequate pumping of blood from the heart, causing a backup of fluid in the pulmonary circulation. This fluid accumulation in the alveoli (air sacs) of the lungs hinders gas exchange, resulting in the characteristic shortness of breath.
An illustration would depict the heart, lungs, and blood vessels, highlighting the path of blood flow and the location of fluid accumulation. A cross-section of the lung would demonstrate the alveolar spaces filled with fluid, diminishing the capacity for oxygen uptake.
A Patient’s Experience with PND
“The first time it happened, I thought I was having a heart attack. I woke up gasping for air, my chest felt tight, and I couldn’t get comfortable. It was terrifying. The episodes were often triggered by lying down, and I’d have to sit up or stand to breathe easier. This significantly impacted my sleep, leading to fatigue and irritability during the day.
It also affected my ability to participate in daily activities, such as walking or playing with my grandchildren. I felt isolated and worried about the future, but the treatment has helped me regain control of my life.”
Chest X-Ray Findings in a Patient with PND, Paroxysmal nocturnal dyspnea pnd
A chest X-ray in a patient with PND would reveal signs of pulmonary edema. The characteristic findings would include an overall increase in the opacity of the lung fields, particularly in the lower lung zones. There might be a hazy appearance to the lung tissue, and the vascular markings might be more prominent than usual. The heart silhouette might also appear enlarged.
In summary, the x-ray would show fluid buildup in the alveoli, evident as increased opacity and haziness, primarily in the lower lung fields, accompanied by a potential cardiac enlargement.
Conclusive Thoughts
In conclusion, paroxysmal nocturnal dyspnea (PND) is a significant health concern demanding comprehensive understanding and effective management. By recognizing the underlying causes, symptoms, and potential complications, individuals can work with healthcare professionals to develop personalized strategies for diagnosis, treatment, and prevention. Early intervention and a proactive approach are key to minimizing the impact of PND on quality of life.










