Primary dysmenorrhea in teenagers is a common experience, marked by painful cramps during menstruation. This comprehensive guide explores the causes, symptoms, and management strategies for this often debilitating condition, empowering teenagers and their families to navigate this challenging period with greater understanding and support. We’ll delve into the physiological mechanisms, prevalence, and impact on daily life.
Understanding the different stages of the menstrual cycle and how symptoms manifest during each phase is crucial for effective management. This article also examines risk factors and potential long-term consequences of untreated dysmenorrhea. We’ll also discuss effective management strategies, from lifestyle modifications to medical interventions, and provide guidance on diagnosis and consultation with healthcare providers.
Defining Primary Dysmenorrhea in Teenagers
Understanding menstrual cramps, particularly in teenagers, is crucial for early intervention and management. Primary dysmenorrhea, the most common type of painful menstruation, significantly impacts a teenager’s quality of life. This often involves intense cramping that interferes with daily activities and school attendance.Primary dysmenorrhea in teenagers is characterized by painful menstrual cramps that are not caused by an underlying medical condition.
The pain typically arises from uterine contractions, which are essential for shedding the uterine lining. However, in teenagers with primary dysmenorrhea, these contractions are more intense and prolonged than in those without the condition. This heightened intensity often leads to a range of uncomfortable symptoms.
Physiological Mechanisms of Pain
The physiological mechanisms behind primary dysmenorrhea in teenagers center on the release of prostaglandins, chemicals that trigger uterine contractions. Increased prostaglandin levels stimulate the uterus to contract more forcefully, leading to the intense pain associated with cramps. This process is often exacerbated in teenagers whose bodies are still developing and whose hormonal balances are adjusting. Additionally, the decreased production of uterine blood flow can cause ischemia and trigger pain signals to the brain.
Symptoms and Characteristics
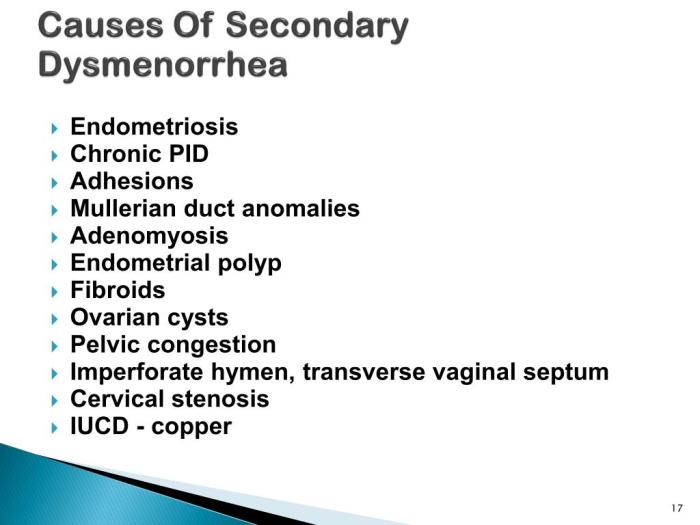
Differentiating primary dysmenorrhea from other conditions like endometriosis or pelvic inflammatory disease is crucial for proper diagnosis and treatment. While both conditions may present with pelvic pain, the underlying causes and accompanying symptoms often differ. Primary dysmenorrhea is typically associated with menstrual cramps, whereas other conditions may involve other symptoms, such as unusual vaginal discharge or fever. It is important to seek medical attention if symptoms beyond typical menstrual cramps are present.
Stages of Menstrual Cycle and Symptoms
Understanding how symptoms manifest throughout the menstrual cycle can aid in recognizing patterns and managing discomfort. The following table Artikels typical symptoms experienced by teenagers during different stages.
| Menstrual Cycle Stage | Typical Symptoms |
|---|---|
| Premenstrual Phase (Days 1-7 before menstruation) | Mild lower abdominal discomfort, bloating, mood swings, breast tenderness, fatigue |
| Menstrual Phase (Days 1-7 of menstruation) | Severe lower abdominal cramping, radiating pain to the back or thighs, nausea, vomiting, headache, diarrhea, fatigue |
| Postmenstrual Phase (Days 7-14 after menstruation) | Gradually decreasing pain and discomfort, normalization of symptoms |
Prevalence and Risk Factors
Primary dysmenorrhea, the painful menstruation experienced by many teenagers, isn’t just a universal teenage experience. Understanding its prevalence and the factors that contribute to its occurrence is crucial for effective management and support. This knowledge empowers both teens and healthcare providers to address the condition proactively.
Prevalence of Primary Dysmenorrhea
Primary dysmenorrhea affects a significant portion of menstruating teenagers globally. Studies show a wide range of prevalence, with estimates varying considerably based on factors such as the methodology used for the study, the population sampled, and the specific definition of dysmenorrhea. While exact figures remain elusive, prevalence is generally higher in younger age groups and often decreases with age.
There might be regional variations in prevalence due to differing dietary habits, cultural norms, and access to healthcare. For instance, a study in North America might yield different prevalence rates compared to a study in South Asia.
Risk Factors Associated with Primary Dysmenorrhea
Several risk factors contribute to the development and severity of primary dysmenorrhea in teenagers. Genetics, diet, and lifestyle choices play significant roles in modulating the intensity and duration of menstrual pain. Environmental factors may also play a role, though the exact mechanisms are still being investigated.
Genetic Factors
A family history of dysmenorrhea is a known risk factor. The genetic predisposition to certain hormonal imbalances and sensitivities may influence the severity and frequency of menstrual pain. The inheritance pattern is complex and not fully understood, but studies suggest a potential link to genes related to prostaglandin production and uterine contractility.
Dietary Factors
Dietary habits can significantly impact menstrual health. A diet lacking in essential nutrients or high in processed foods and unhealthy fats may exacerbate symptoms. Conversely, a balanced diet rich in fruits, vegetables, and whole grains may contribute to a healthier menstrual cycle and reduce the risk of dysmenorrhea. For example, diets high in saturated fats might increase inflammation, which could contribute to painful menstruation.
Lifestyle Factors
Lifestyle choices, such as stress levels, physical activity, and sleep patterns, can also affect the severity of dysmenorrhea. High levels of stress can increase hormonal fluctuations and muscle tension, leading to more intense pain. Lack of physical activity or poor sleep hygiene might negatively impact overall well-being, which could indirectly influence menstrual symptoms. For example, regular exercise can often improve overall health and well-being, and this positive effect may reduce the intensity of menstrual pain in some cases.
Comparison Across Ethnic Groups and Socioeconomic Backgrounds
Studies on the prevalence and severity of primary dysmenorrhea across different ethnic groups and socioeconomic backgrounds are limited and often lack detailed data. Available evidence suggests that variations might exist, but definitive conclusions remain elusive. Factors like access to healthcare, cultural norms regarding menstrual health, and overall health and well-being could contribute to these potential disparities. Further research is needed to fully understand these variations.
Dealing with primary dysmenorrhea as a teenager can be tough, those throbbing cramps can really throw you off. Sometimes, these intense menstrual pains can mimic other conditions, like a migraine without aura. Understanding the differences is key, and learning about what a migraine without aura is can help you pinpoint the source of your discomfort what is a migraine without aura.
Ultimately, though, remembering that primary dysmenorrhea is a common and treatable condition is important. Knowing the difference between the two can help you navigate your symptoms and get the right support.
Summary Table of Risk Factors
| Category | Risk Factor | Description |
|---|---|---|
| Genetic Factors | Family history of dysmenorrhea | Presence of dysmenorrhea in close family members increases risk. |
| Dietary Factors | High intake of processed foods | Processed foods can lead to inflammation and hormonal imbalances. |
| Dietary Factors | Low intake of fruits and vegetables | Lack of essential nutrients can impact overall health, potentially worsening symptoms. |
| Lifestyle Factors | High stress levels | Stress can increase hormonal fluctuations and muscle tension, leading to more intense pain. |
| Lifestyle Factors | Lack of regular exercise | Physical inactivity can negatively impact overall health and well-being. |
| Lifestyle Factors | Poor sleep hygiene | Insufficient or poor-quality sleep can exacerbate symptoms. |
Impact on Adolescent Life
Dealing with primary dysmenorrhea can significantly impact a teenager’s daily life, affecting everything from school performance to social interactions and overall well-being. The pain and discomfort associated with this condition can disrupt their routines and make it challenging to participate fully in activities they enjoy. Understanding these effects is crucial for providing appropriate support and management strategies.The intense cramping and accompanying symptoms of primary dysmenorrhea can make it difficult for teenagers to concentrate in school, leading to decreased academic performance.
Missing classes due to pain or needing to take frequent breaks can also hinder their learning progress. Furthermore, the emotional distress associated with the condition can affect their ability to engage in social activities and maintain healthy relationships.
Impact on School Performance
The pain and discomfort associated with primary dysmenorrhea can significantly impact a teenager’s ability to focus and perform well in school. Frequent absences, missed classes, and difficulty concentrating can all contribute to lower grades and decreased academic achievement. Some teenagers may struggle to participate actively in class discussions or complete assignments on time due to their pain. This can lead to feelings of inadequacy and anxiety about their academic performance.
Impact on Social Activities
Primary dysmenorrhea can limit a teenager’s participation in social activities. The pain and discomfort can make it difficult to engage in physical activities, participate in extracurriculars, or attend social events. This can lead to feelings of isolation and exclusion from peer groups. A teenager might withdraw from social interactions to avoid discomfort or embarrassment related to their symptoms.
This can also affect their self-confidence and social skills development.
Impact on Emotional Health and Mental State
Primary dysmenorrhea can have a significant impact on a teenager’s emotional health and mental state. The persistent pain and associated symptoms can trigger anxiety, irritability, and mood swings. These emotional responses can further exacerbate the pain and create a vicious cycle. The experience can be overwhelming and lead to feelings of frustration, hopelessness, and even depression. Teenagers might experience difficulty coping with the emotional distress alongside their physical symptoms.
Impact on Self-Image and Body Perception
The experience of primary dysmenorrhea can influence a teenager’s self-image and body perception. The persistent pain and discomfort can lead to feelings of shame or embarrassment about their bodies, especially during periods of intense cramping. This can affect their self-esteem and confidence, and create negative associations with menstruation. Some teenagers may internalize the pain as a reflection of their own worth or inadequacy, leading to a negative body image and impacting their overall well-being.
Potential Long-Term Consequences, Primary dysmenorrhea in teenagers
Untreated or poorly managed primary dysmenorrhea can have potential long-term consequences. Chronic pain can affect a teenager’s ability to focus on their studies and pursue extracurricular activities. The emotional distress can potentially lead to more severe mental health issues, such as anxiety or depression, if not addressed appropriately. Furthermore, the impact on social life could lead to difficulties in forming and maintaining relationships.
Ugh, those awful cramps! Primary dysmenorrhea in teenagers can be a real pain, literally. It’s so frustrating when you’re just trying to get through the day, and you’re constantly wondering why you keep feeling under the weather. Are you experiencing other symptoms? If so, checking out this resource on why do I keep getting sick might help you figure out what’s going on.
It’s important to remember that while primary dysmenorrhea is common, it’s definitely something to discuss with your doctor if the pain is severe or interferes with your daily life.
It’s important to recognize and address this issue promptly to prevent long-term complications.
Management Strategies and Treatments
Navigating painful periods as a teenager can be challenging. Fortunately, effective management strategies exist, ranging from simple lifestyle adjustments to more involved medical interventions. Understanding these options empowers teenagers to take control of their menstrual health and experience relief from discomfort.Effective management strategies for primary dysmenorrhea often involve a combination of approaches tailored to individual needs. A multifaceted approach, incorporating lifestyle modifications, over-the-counter pain relievers, and potentially hormonal contraceptives, can significantly improve a teenager’s quality of life during menstruation.
Dealing with primary dysmenorrhea as a teenager can be tough, with cramps often disrupting daily life. Interestingly, similar to managing painful periods, maintaining a healthy weight can significantly impact overall well-being, including potentially reversing type 2 diabetes. Finding ways to achieve a healthy weight, like those discussed in weight loss reverse type 2 diabetes , could actually help alleviate some of the symptoms associated with primary dysmenorrhea in the long run.
Focusing on a balanced diet and regular exercise might be beneficial for both.
Lifestyle Modifications
Adopting healthy habits can play a crucial role in mitigating dysmenorrhea symptoms. Regular exercise, a balanced diet, and stress management techniques can positively influence the hormonal fluctuations associated with menstruation. Maintaining a consistent sleep schedule and reducing stress through relaxation exercises, like yoga or meditation, can contribute to overall well-being and potentially alleviate period pain. Dietary changes, such as incorporating foods rich in anti-inflammatory compounds, might also help.
Over-the-Counter Pain Relievers
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, are commonly used to manage mild to moderate pain associated with primary dysmenorrhea. These medications work by reducing inflammation and prostaglandin production, thereby decreasing the intensity of menstrual cramps. Dosage and frequency should always be in accordance with the product instructions. It is crucial to consult with a healthcare provider before taking any new medication, especially if the teenager has pre-existing health conditions or allergies.
Hormonal Contraceptives
Hormonal contraceptives, including birth control pills, patches, and rings, can effectively manage primary dysmenorrhea in teenagers. These methods often reduce menstrual flow and prostaglandin production, leading to decreased pain and cramping. The use of hormonal contraceptives is typically discussed with a healthcare provider, who can assess individual needs and potential benefits and risks. The choice of hormonal contraceptive should consider factors like potential side effects, desired protection against pregnancy, and overall health.
Comparison of Treatment Options
Different treatment options for primary dysmenorrhea offer varying degrees of effectiveness and potential side effects. A healthcare provider can help teenagers weigh the pros and cons of each approach based on their specific situation.
| Method | Effectiveness | Potential Side Effects |
|---|---|---|
| Lifestyle Modifications | Moderate to High (depending on individual response and consistency) | Generally minimal, but may require lifestyle changes that may not be suitable for all teenagers. |
| Over-the-Counter Pain Relievers (NSAIDs) | High (for mild to moderate pain) | Possible gastrointestinal upset (e.g., nausea, heartburn), allergic reactions, or interactions with other medications. |
| Hormonal Contraceptives | High (often reduces menstrual flow and pain) | Potential side effects include mood changes, headaches, breast tenderness, and, in rare cases, blood clots. Not suitable for all individuals. |
Diagnosis and Consultation: Primary Dysmenorrhea In Teenagers
Navigating the complexities of primary dysmenorrhea can feel overwhelming, especially for teenagers. Understanding the diagnostic process and the crucial role of open communication with healthcare providers is key to effective management and relief. This phase involves more than just a quick fix; it’s about a thorough understanding of the individual’s experience and needs.A comprehensive evaluation of primary dysmenorrhea involves a detailed medical history, physical examination, and potentially, further diagnostic tests.
This process aims to rule out other conditions with similar symptoms and ensure an accurate diagnosis. The focus is on providing personalized care that addresses the unique needs of each adolescent.
The Diagnostic Process
A thorough medical history is paramount in diagnosing primary dysmenorrhea. This includes detailed information about the menstrual cycle, pain characteristics (severity, duration, location), associated symptoms (nausea, vomiting, fatigue), and any family history of menstrual problems. Understanding the timing and patterns of pain can be critical to distinguish it from other potential conditions. Factors like the age of menarche (first period) and the duration of menstrual cycles are also important considerations.
The Role of the Healthcare Provider
Healthcare providers play a vital role in guiding teenagers through the diagnostic process and developing an effective management plan. They act as a trusted source of information and support, ensuring the teenager feels comfortable discussing their symptoms and concerns. This includes providing accurate information about primary dysmenorrhea, addressing anxieties, and fostering a safe space for open communication. A healthcare provider should also consider potential psychological factors, which can influence pain perception and response.
Importance of Open Communication
Open and honest communication between teenagers and healthcare professionals is crucial for successful diagnosis and management of primary dysmenorrhea. Teenagers should feel empowered to express their concerns, ask questions, and share their experiences without judgment. Healthcare providers should create an environment where teenagers feel comfortable discussing their menstrual health, including any discomfort or challenges they might be facing.
This open dialogue helps to build trust and facilitate a shared understanding of the condition.
Questions for a Doctor
A teenager seeking advice about primary dysmenorrhea should be prepared to ask relevant questions to ensure a clear understanding of their condition and available treatment options. This proactive approach fosters collaboration and enables informed decision-making. The following list provides examples of questions a teenager might ask:
- What are the possible causes of my pain?
- What are the different types of pain management options available?
- What is the long-term outlook for my condition?
- Are there any lifestyle changes I can make to help manage my pain?
- How can I better understand my menstrual cycle?
- Are there any other conditions that might have similar symptoms?
- What are the potential side effects of the prescribed medications?
- Can you recommend any resources or support groups for teenagers with similar experiences?
- How often should I follow up for check-ups?
These questions demonstrate a proactive approach to understanding and managing their condition. Asking these questions empowers teenagers to take an active role in their healthcare, leading to better outcomes.
Preventive Measures
Navigating the challenges of primary dysmenorrhea in adolescence often involves proactive strategies to minimize discomfort and improve overall well-being. Implementing preventive measures alongside medical treatments can significantly enhance the quality of life for teenagers experiencing painful menstruation. These proactive steps focus on lifestyle adjustments, dietary choices, and stress management techniques to support the body’s natural responses.A holistic approach to managing primary dysmenorrhea involves recognizing the interconnectedness of physical and emotional health.
Understanding the potential contributing factors, such as inflammation, hormonal fluctuations, and stress levels, allows for targeted interventions. By incorporating preventive measures into daily routines, teenagers can potentially reduce the severity and frequency of painful periods, empowering them to actively participate in their well-being.
Healthy Lifestyle Choices
A healthy lifestyle forms the foundation for managing primary dysmenorrhea. Maintaining a balanced diet, engaging in regular exercise, and practicing stress-reduction techniques are crucial for overall well-being and can positively impact menstrual health. These practices are not merely preventative measures but rather essential components of a healthy lifestyle that benefit all aspects of adolescent development.
- Balanced Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins provides essential nutrients for optimal hormonal balance and overall health. Nutrient deficiencies can contribute to various health issues, including menstrual irregularities. A balanced diet supports the body’s natural processes, reducing the potential for inflammatory responses and improving the body’s ability to manage hormonal fluctuations.
- Regular Exercise: Regular physical activity promotes blood circulation and helps regulate hormone levels. Exercise also contributes to stress reduction, which can play a role in alleviating dysmenorrhea symptoms. Moderate-intensity exercises, such as brisk walking, swimming, or cycling, can effectively reduce discomfort associated with menstruation.
- Stress Management: Chronic stress can exacerbate menstrual pain. Implementing stress-reducing techniques, such as yoga, meditation, deep breathing exercises, or spending time in nature, can significantly impact the body’s response to hormonal changes. Stress management techniques are not only beneficial for menstrual health but also for overall mental and emotional well-being.
Dietary Recommendations
Certain dietary choices can potentially contribute to a reduction in dysmenorrhea symptoms. Foods rich in anti-inflammatory properties, such as omega-3 fatty acids and antioxidants, might help mitigate the inflammatory responses that often accompany menstruation. Incorporating these foods into a balanced diet can have a positive impact on menstrual health and reduce overall discomfort.
- Omega-3 Fatty Acids: Foods rich in omega-3 fatty acids, like fatty fish (salmon, tuna), flaxseeds, and chia seeds, may help reduce inflammation. These healthy fats support the body’s natural processes and contribute to a balanced inflammatory response.
- Antioxidant-Rich Foods: Fruits and vegetables rich in antioxidants, such as berries, citrus fruits, and leafy greens, can support the body’s natural defenses against oxidative stress. These foods can contribute to overall health and may help mitigate discomfort associated with menstruation.
- Foods to Limit: Excessive intake of processed foods, sugary drinks, and caffeine may worsen inflammation. Reducing the consumption of these items may contribute to a reduction in dysmenorrhea symptoms.
Importance of a Balanced Diet for Menstrual Health
A balanced diet is essential for maintaining overall health and plays a significant role in menstrual health. A diet rich in essential nutrients supports hormonal balance, regulates the menstrual cycle, and contributes to the overall well-being of the adolescent. Maintaining a healthy weight, alongside a balanced diet, can contribute to a smoother menstrual cycle.
- Nutrient Support: A balanced diet provides the essential nutrients required for proper hormonal function and reducing inflammation. Sufficient intake of vitamins, minerals, and proteins supports the body’s natural processes during menstruation.
- Hormonal Regulation: Nutrients in a balanced diet contribute to the regulation of hormones, which is crucial for maintaining a regular and healthy menstrual cycle. Nutrient deficiencies can disrupt hormonal balance and potentially lead to dysmenorrhea.
- Impact on Inflammation: A balanced diet rich in anti-inflammatory foods may help reduce inflammation, which is often associated with painful periods. Foods with anti-inflammatory properties can positively impact menstrual health and reduce discomfort.
Wrap-Up
In conclusion, primary dysmenorrhea in teenagers requires a multifaceted approach that addresses the physical, emotional, and social aspects of the condition. This article provides a comprehensive overview of the topic, from understanding the underlying mechanisms to practical management strategies. By empowering teenagers with knowledge and support, we can help them navigate this challenging phase of their lives with greater ease and well-being.
Remember, open communication with healthcare professionals is key.









