Pustular rash types treatment encompasses a wide range of skin conditions, from acne to psoriasis, each with its own unique characteristics and treatment strategies. Understanding the various types of pustular rashes, their triggers, and the underlying mechanisms is crucial for effective diagnosis and management. This guide delves into the intricacies of pustular rash types treatment, providing a comprehensive overview of the diagnostic process, treatment options, and patient management strategies.
This detailed exploration covers everything from the initial identification of different pustular rash types to the management of potential complications. We will explore the importance of a thorough patient history and physical examination, discuss various diagnostic tests, and analyze the specific treatment approaches for each type of pustular rash. The guide also emphasizes patient education and follow-up care, ultimately aiming to empower individuals with pustular rashes to effectively manage their condition.
Introduction to Pustular Rashes
Pustular rashes are skin conditions characterized by the presence of pus-filled blisters, or pustules. These eruptions can vary significantly in size, shape, and distribution across the skin, ranging from tiny, localized pustules to larger, more widespread lesions. Understanding the diverse causes and clinical presentations of pustular rashes is crucial for accurate diagnosis and effective treatment.Pustular rashes can stem from a wide array of underlying conditions, from simple infections to more complex systemic diseases.
Categorizing these rashes based on their causes or clinical appearance provides a framework for understanding their origins and appropriate management. Common triggers and risk factors, such as bacterial infections, certain medications, and underlying medical conditions, will be explored in the following sections. Furthermore, we will discuss the mechanisms that contribute to the development of these inflammatory skin lesions.
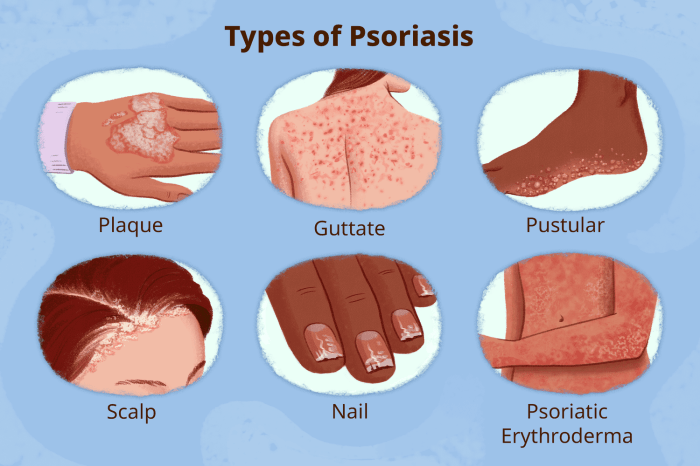
Types of Pustular Rashes
Pustular rashes manifest in various forms, each with unique characteristics. They are categorized based on the underlying cause or the clinical presentation. Examples include acne, impetigo, and psoriasis, among others. The diverse nature of these conditions underscores the importance of a thorough examination and patient history to pinpoint the specific cause.
Common Triggers and Risk Factors
Several factors can contribute to the development of pustular rashes. Infections, such as bacterial or fungal infections, are common triggers. Certain medications, both over-the-counter and prescription, can induce pustular eruptions as a side effect. Underlying medical conditions, like psoriasis or inflammatory bowel disease, can also increase the risk of developing pustular rashes. Genetic predisposition, age, and environmental factors may also play a role.
Underlying Mechanisms
The development of pustular rashes often involves an interplay of factors. Infections can trigger an inflammatory response, leading to the accumulation of neutrophils and the formation of pus. Certain medications may directly irritate the skin or disrupt the immune system, increasing the susceptibility to rashes. Chronic inflammatory conditions like psoriasis may result in abnormal immune responses, leading to skin lesions.
The precise mechanisms responsible for pustular rashes remain complex and subject to ongoing research.
Comparison of Clinical Presentations
| Rash Type | Appearance | Distribution | Associated Symptoms |
|---|---|---|---|
| Acne | Comedones (blackheads/whiteheads), papules, pustules, nodules, cysts | Mostly on face, back, chest | Pain, redness, tenderness, scarring |
| Impetigo | Small, superficial, honey-colored crusts over vesicles and pustules | Usually on face, extremities | Itching, pain, fever, malaise |
| Psoriasis | Red, scaly plaques with silvery-white scales, pustules sometimes present | Can occur anywhere on the body | Itching, burning, pain, joint pain (psoriatic arthritis) |
This table provides a simplified overview of the clinical presentations. Individual cases may exhibit variations depending on the specific cause and severity of the rash. Accurate diagnosis requires a comprehensive evaluation by a healthcare professional.
Diagnostic Considerations
Pinpointing the specific cause of a pustular rash is crucial for effective treatment. Accurate diagnosis relies on a meticulous approach, combining patient history, physical examination, and potentially, diagnostic testing. This process helps distinguish between various conditions, each requiring tailored therapeutic interventions.The diagnostic journey for pustular rashes often begins with a thorough understanding of the patient’s medical history. Factors like recent illnesses, medications, allergies, and exposure to potential irritants or pathogens play significant roles in identifying the possible culprit.
Treating pustular rashes can be tricky, involving various approaches depending on the type. Learning how to properly use a glucometer, for example, is crucial for managing certain conditions that can manifest as pustular rashes. Understanding the proper technique for taking blood sugar readings with how to use a glucometer is vital for accurate diagnoses and effective treatment plans, which are essential for managing these types of skin conditions.
Ultimately, proper diagnosis and treatment of pustular rashes are key to finding relief.
A detailed description of the rash’s appearance, including its location, duration, and associated symptoms, is also essential.
Patient History and Physical Examination
A comprehensive patient history is vital for narrowing down potential causes. Questions regarding recent travel, exposure to sick contacts, or use of new medications or topical products can help determine if an infectious or allergic etiology is more likely. The physical examination is equally important, allowing for direct observation of the rash’s characteristics, such as distribution, size, color, and any associated lesions.
Dealing with pustular rash types can be tricky, and understanding the underlying causes is key to effective treatment. Sometimes, deficiencies in essential nutrients, like vitamins, can play a role. Learning more about vitamins and how they function in the body can be really helpful. For example, vitamins what are they and how do they work can shed light on the importance of a balanced diet for overall health, which can indirectly influence the treatment of pustular rashes.
Ultimately, a holistic approach, considering both external and internal factors, is often the most effective strategy for managing these skin conditions.
The presence of accompanying symptoms like fever, pain, or systemic manifestations (e.g., joint pain) can provide further clues to the underlying condition.
Treating pustular rash types often involves addressing the underlying cause. Sometimes, systemic conditions like rheumatoid arthritis require specific treatments, such as DMARDs for rheumatoid arthritis. DMARDs for rheumatoid arthritis can be crucial in managing the inflammation, which can contribute to the rash. Ultimately, the best approach to pustular rash types treatment depends on a thorough diagnosis and individualized care plan.
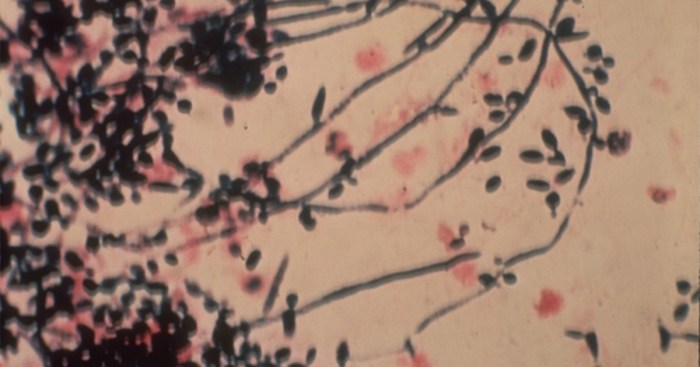
Role of Diagnostic Tests
Various diagnostic tests can aid in identifying the specific cause of a pustular rash. Skin biopsies are often employed to examine skin tissue microscopically, revealing cellular changes indicative of certain conditions. Cultures can determine if bacteria, fungi, or other microorganisms are present, guiding treatment with targeted antibiotics or antifungals. In some cases, blood tests may be necessary to assess for systemic inflammatory markers or specific autoimmune conditions that might contribute to the rash.
Diagnostic Criteria for Different Pustular Rash Types
The diagnostic criteria for different pustular rash types vary depending on the suspected underlying condition. For example, in cases of acne vulgaris, the presence of comedones (blackheads and whiteheads), inflammatory papules, and pustules, often with a characteristic distribution on the face, back, and chest, typically leads to a diagnosis. However, in cases of pustular psoriasis, the rash might exhibit a distinct pattern of erythema and scaling, accompanied by numerous sterile pustules, often affecting the extensor surfaces of the limbs.
Table of Diagnostic Steps for Common Pustular Rash Types
| Rash Type | Patient History Focus | Physical Examination Focus | Diagnostic Tests | Diagnostic Criteria |
|---|---|---|---|---|
| Acne Vulgaris | Recent medications, topical products, diet, stress levels | Comedones, papules, pustules, distribution | Skin biopsy (less commonly), cultures (less commonly) | Presence of comedones, inflammatory lesions, characteristic distribution |
| Pustular Psoriasis | History of psoriasis, recent stress, medications | Erythema, scaling, pustules, distribution (extensor surfaces) | Skin biopsy, blood tests for inflammatory markers | Presence of pustules, erythema, scaling, characteristic distribution |
| Bacterial Folliculitis | Recent skin trauma, exposure to contaminated surfaces | Small, superficial pustules, often grouped, erythema | Skin cultures | Presence of superficial pustules, localized infection |
Treatment Strategies for Specific Pustular Rash Types
Pustular rashes, characterized by the presence of pus-filled blisters, can arise from various underlying conditions. Effective treatment hinges on accurate diagnosis to target the root cause. Different treatment strategies are employed depending on the specific type of pustular rash, whether acne-related, associated with psoriasis, impetigo, or drug reactions. This section will delve into the primary treatment approaches for each type.Understanding the diverse causes of pustular rashes is crucial for successful management.
For instance, acne-related pustules often respond well to topical treatments, while pustular psoriasis might necessitate systemic medications for control. Similarly, impetigo requires prompt antibiotic therapy, and drug-induced pustules necessitate discontinuation of the offending agent.
Acne-Related Pustular Rashes
Topical treatments are frequently the first line of defense for acne-related pustular rashes. These treatments aim to reduce inflammation, control bacteria, and promote skin healing. Topical retinoids, such as tretinoin, can exfoliate the skin, unclog pores, and decrease inflammation. Benzoyl peroxide is another common topical agent that helps kill bacteria and reduce inflammation. In more severe cases, topical antibiotics, like clindamycin or erythromycin, may be prescribed to combat bacterial overgrowth.
Oral antibiotics, such as tetracycline or doxycycline, might be necessary for persistent or extensive acne. In some cases, oral isotretinoin (Accutane) is considered for severe, recalcitrant acne.
Pustular Psoriasis
Pustular psoriasis, a more severe form of the condition, often requires a multi-pronged approach. Topical corticosteroids, such as betamethasone, can be effective in reducing inflammation. Topical vitamin D analogs, like calcipotriene, can help regulate the immune system. Systemic medications, such as methotrexate or cyclosporine, are frequently used for more severe cases to control the inflammatory response. Biological therapies targeting specific inflammatory pathways, such as TNF-alpha inhibitors, may be considered in patients who don’t respond to other treatments.
Phototherapy, such as ultraviolet B (UVB) light therapy, can also be effective in managing pustular psoriasis.
Impetigo-Related Pustular Rashes
Impetigo, a highly contagious bacterial skin infection, requires prompt antibiotic treatment. Topical antibiotics, such as mupirocin, can be effective for localized infections. Oral antibiotics, such as penicillin or cephalosporins, are often necessary for more extensive or severe cases. Early intervention is crucial to prevent the spread of infection. Strict hygiene measures, including handwashing, are essential to prevent further transmission.
Pustular Drug Eruptions
Pustular drug eruptions are often a reaction to a medication. The primary treatment strategy is to discontinue the offending medication immediately. Supportive care, such as topical corticosteroids or antihistamines, may be used to manage symptoms like itching and inflammation. In severe cases, systemic corticosteroids might be considered to reduce inflammation. Identifying the causative drug is crucial for preventing future eruptions.
Treatment Options for Different Pustular Rash Types
| Rash Type | Medication Class | Examples & Dosages (Typical) |
|---|---|---|
| Acne | Topical Retinoids | Tretinoin 0.025-0.1% cream/gel |
| Acne | Antibiotics | Clindamycin 1% topical lotion/solution, Doxycycline 100mg twice daily |
| Pustular Psoriasis | Topical Corticosteroids | Betamethasone valerate 0.1% ointment |
| Pustular Psoriasis | Systemic DMARDs | Methotrexate 7.5-20mg weekly |
| Impetigo | Topical Antibiotics | Mupirocin 2% ointment |
| Impetigo | Oral Antibiotics | Penicillin V 250mg 4 times daily |
| Drug Eruptions | Discontinue offending medication | Stop the causative drug immediately |
Patient Management and Education
Effective patient management for pustular rashes hinges on thorough education and support. Understanding the disease course, treatment protocols, and potential side effects empowers patients to actively participate in their care, leading to improved outcomes and adherence to treatment plans. This proactive approach is crucial for managing the condition effectively and preventing complications.
Importance of Patient Education
Patient education is paramount in managing pustular rashes. Providing clear, concise information about the disease’s nature, expected course, and potential complications empowers patients to make informed decisions and actively participate in their care. Education should address the specific type of pustular rash, its triggers (if known), and the rationale behind the chosen treatment. This knowledge empowers patients to recognize early warning signs, understand the importance of adherence, and manage potential side effects proactively.
Adherence to Treatment Regimens
Adherence to prescribed treatment regimens is critical for successful pustular rash management. Non-adherence can lead to treatment failure, disease progression, and potential complications. To encourage adherence, clinicians should explain the rationale behind each treatment step, addressing potential concerns and questions. Clear communication, tailored explanations, and practical strategies for incorporating treatment into daily routines can significantly improve adherence rates.
Managing Potential Side Effects
Pustular rash treatments can sometimes produce side effects. Educating patients about potential side effects, their typical presentation, and strategies for managing them is crucial. For example, some treatments may cause skin irritation, dryness, or itching. Providing guidance on managing these symptoms, such as using emollients or mild topical corticosteroids, can prevent discomfort and ensure treatment continuation.
Importance of Follow-Up Appointments
Regular follow-up appointments are essential for monitoring treatment efficacy and adjusting strategies as needed. These appointments allow clinicians to assess treatment response, identify any emerging complications, and modify the treatment plan accordingly. This proactive approach ensures that the treatment remains effective and minimizes potential long-term consequences. Early detection of treatment failure or adverse events is crucial for timely intervention.
Patient Education Materials, Pustular rash types treatment
| Pustular Rash Type | Key Educational Points |
|---|---|
| Acne Vulgaris (with pustules) | Importance of hygiene, avoiding harsh scrubs, managing stress, appropriate topical treatments, and the potential role of oral medications. |
| Pustular psoriasis | Recognizing triggers (stress, infections, medications), importance of maintaining skin hydration, topical therapies, and the potential role of systemic medications. |
| Acute Generalized Exanthematous Pustulosis (AGEP) | Recognition of the abrupt onset, avoidance of potential triggers (medications), and importance of prompt medical attention. |
| Subcorneal pustular dermatosis | Understanding the chronic nature of the disease, importance of consistent topical treatments, and potential need for systemic medications. |
This table provides a concise overview of key educational points for various pustular rash types. Clinicians should tailor their explanations to the specific condition and individual patient needs, addressing their concerns and questions to ensure complete understanding.
Complications and Prognosis: Pustular Rash Types Treatment
Untreated or inadequately managed pustular rashes can lead to a range of complications, impacting both short-term and long-term well-being. Understanding the potential complications and the factors influencing prognosis is crucial for effective patient management. Different types of pustular rashes exhibit varying degrees of severity and potential for complications, necessitating tailored treatment strategies.The long-term prognosis for various pustular rashes is influenced by numerous factors, including the underlying cause, the severity of the rash, and the effectiveness of treatment.
Early diagnosis and prompt, appropriate treatment are essential in minimizing complications and improving the patient’s quality of life. Factors such as adherence to treatment plans and timely follow-up appointments also play a significant role in achieving favorable outcomes.
Potential Complications of Untreated Pustular Rashes
Untreated or inadequately managed pustular rashes can lead to several complications, ranging from minor skin concerns to more serious systemic issues. These complications can affect various aspects of a patient’s health and well-being.
- Skin Damage and Scarring: Prolonged or severe pustular rashes can cause significant skin damage, including ulceration, crusting, and permanent scarring. The extent of scarring depends on the severity and duration of the rash, as well as the individual’s healing response. For example, extensive and untreated acne vulgaris can result in noticeable and permanent scarring, affecting self-esteem and potentially requiring cosmetic procedures.
- Secondary Infections: Open sores and lesions associated with pustular rashes create entry points for bacteria, leading to secondary infections. These infections can range from superficial skin infections to more serious systemic infections. Prompt and appropriate treatment of the underlying rash, as well as vigilant hygiene practices, are crucial in preventing secondary infections.
- Systemic Involvement: Some types of pustular rashes, like pustular psoriasis, can manifest systemic symptoms and potentially impact other organ systems. In such cases, prompt medical intervention is necessary to manage the systemic manifestations and prevent complications.
- Psychological Impact: The aesthetic and functional consequences of pustular rashes can have a significant psychological impact on individuals. The emotional distress associated with the appearance of the rash can affect self-esteem, body image, and overall quality of life. Addressing the psychological impact through counseling and support groups can be integral to patient management.
Long-Term Prognosis for Different Pustular Rash Types
The long-term prognosis varies significantly based on the specific type of pustular rash. Factors such as the underlying cause, the severity of the rash, and the effectiveness of treatment all contribute to the overall outcome.
- Pustular psoriasis: The prognosis for pustular psoriasis can vary depending on the severity of the condition. In some cases, the rash may resolve completely, while in others, it may recur. Factors influencing the prognosis include the frequency and severity of flares, response to treatment, and presence of any associated systemic conditions.
- Acne vulgaris: Acne vulgaris typically resolves with appropriate treatment in most cases, but the extent of scarring can vary depending on the severity of the condition and individual factors. Early intervention and consistent treatment are crucial for minimizing the risk of long-term scarring.
- Transient acantholytic dermatosis: Transient acantholytic dermatosis is generally a self-limiting condition, resolving within a few weeks or months. However, recurrence is possible. The prognosis is generally favorable, but it is essential to seek medical attention for appropriate diagnosis and management.
Factors Influencing Prognosis and Potential for Scarring
Several factors influence the prognosis and the potential for scarring associated with pustular rashes. Understanding these factors can help guide treatment strategies and patient management.
- Severity of the rash: The extent and duration of the rash are critical factors. More severe and prolonged rashes tend to have a higher potential for scarring and more extensive complications.
- Underlying medical conditions: Certain medical conditions can influence the course of pustular rashes and their potential for complications. Coexisting conditions may impact the effectiveness of treatment and overall prognosis.
- Treatment response: Prompt and effective treatment is crucial for improving the prognosis and minimizing complications. A positive response to treatment significantly reduces the risk of scarring and other complications.
Preventive Measures to Minimize Complications
Preventive measures play a significant role in reducing the risk of complications associated with pustular rashes. These measures include appropriate treatment, diligent skin care, and addressing any underlying contributing factors.
- Early diagnosis and treatment: Early identification and prompt treatment of pustular rashes are essential for minimizing the risk of complications. This approach helps to limit the duration and severity of the rash.
- Adherence to treatment plans: Patients should meticulously follow their prescribed treatment plan to maximize the effectiveness of therapy. Consistent adherence is crucial for achieving favorable outcomes.
- Proper skin hygiene: Maintaining proper skin hygiene is important to prevent secondary infections and promote healing. Gentle cleansing and appropriate moisturization can support skin health.
Table of Potential Complications and Prognosis of Various Pustular Rash Types
| Pustular Rash Type | Potential Complications | Prognosis (General Overview) |
|---|---|---|
| Pustular psoriasis | Skin damage, scarring, secondary infections, systemic involvement | Variable; can resolve or recur; treatment crucial for favorable outcomes |
| Acne vulgaris | Skin damage, scarring, secondary infections | Usually resolves with treatment; scarring risk varies |
| Transient acantholytic dermatosis | Skin damage, secondary infections | Generally self-limiting; favorable prognosis |
Differential Diagnoses
Pinpointing the exact cause of a pustular rash is crucial for effective treatment. Misdiagnosis can lead to inappropriate therapies and delay in getting the right care. Differentiating pustular rashes from other skin conditions requires careful observation of symptoms, medical history, and potential triggers. This process often involves ruling out various possibilities, including infectious diseases, autoimmune conditions, and even side effects of medications.
Importance of Differentiation
Accurate diagnosis of pustular rashes is paramount for tailoring appropriate treatment. Mistaking a pustular rash for another condition can lead to unnecessary or ineffective interventions, potentially worsening the condition. Prompt and accurate diagnosis ensures the most effective and timely management, minimizing complications and improving patient outcomes. Understanding the distinct features of various skin conditions is essential for successful differentiation.
Comparison with Similar Dermatological Conditions
Pustular rashes can mimic several other skin conditions, necessitating careful evaluation. For example, acne vulgaris often presents with pustules, but its distribution and associated symptoms can differ. Psoriasis, another common skin disorder, can also exhibit pustular formations, but the clinical presentation, including the presence of plaques and scaling, will often provide clues. Dermatitis herpetiformis, characterized by intensely itchy vesicles and papules, can sometimes exhibit a pustular component, but the distinctive morphology and associated systemic symptoms are helpful in distinguishing it.
Key Distinguishing Features
Several key features help differentiate pustular rashes from other dermatological conditions. The location, distribution, and morphology of the pustules; the presence or absence of pruritus (itching); and the patient’s overall health status, including any associated symptoms or medical history, are critical considerations. Furthermore, the timing of the rash’s appearance, along with any possible triggers, like medications or infections, will be important diagnostic elements.
Diagnostic Considerations in Infectious Diseases
Differentiating pustular rashes from infectious diseases is essential for appropriate management. Bacterial infections, like impetigo, present with superficial, honey-colored crusts over the pustules. Fungal infections, such as tinea, often exhibit scaling and erythema around the affected area. Viral infections, like herpes simplex, present with characteristic grouped vesicles or ulcers, which can sometimes be mistaken for pustules. Identifying the causative agent is crucial, as treatment approaches differ significantly.
Table Comparing Pustular Rashes and Differential Diagnoses
| Condition | Pustular Rash Characteristics | Differential Diagnosis Characteristics | Key Distinguishing Features |
|---|---|---|---|
| Acne Vulgaris | Comedones, papules, nodules, often on face, chest, back | Pustules often in a localized pattern, often associated with oily skin | Distribution, presence of comedones, and association with hormonal factors |
| Psoriasis | Erythematous plaques with silvery scales, sometimes with pustules | Plaques and scaling are often prominent, chronic relapsing course | Presence of plaques, scaling, and history of flares |
| Dermatitis Herpetiformis | Intensely itchy vesicles and papules, sometimes with pustules | Pruritic vesicles, grouped lesions, associated with celiac disease | Intense pruritus, distribution, and association with systemic conditions |
| Impetigo | Superficial pustules that rupture and form honey-colored crusts | Rapidly spreading, superficial infection, often in children | Appearance of crusts, rapid spread, and bacterial culture |
| Tinea | Pustules, scaling, erythema, often in specific locations | Fungal infection, characteristic scaling and ring-like lesions | Characteristic scaling pattern, fungal culture results |
Case Studies and Illustrations
Diving deeper into the realm of pustular rashes, understanding real-world cases is crucial for refining diagnostic accuracy and treatment efficacy. These case studies highlight the complexities of these skin conditions, showcasing the diverse presentations and responses to various treatment approaches. They also illustrate the importance of meticulous observation and careful consideration of patient history and factors.
A Case Study of Acne Conglobata
This case involved a 22-year-old male presenting with a progressively worsening, painful, and extensive pustular rash primarily affecting his back and chest. The patient reported worsening symptoms over the past six months, including significant pain and discomfort, which interfered with daily activities. Initial examination revealed numerous large, deep, and interconnected pustules, along with significant inflammation and scarring. The patient had a history of mild acne vulgaris in adolescence, but this presentation was considerably more severe.The diagnostic process included a thorough history, physical examination, and relevant laboratory tests.
The clinical presentation strongly suggested acne conglobata, a severe form of acne characterized by large, inflamed pustules, nodules, and often scarring. Further investigations, including skin biopsies, were performed to rule out other conditions.Treatment focused on controlling inflammation, reducing bacterial load, and managing pain. A combination of topical and systemic therapies was employed, including benzoyl peroxide, topical retinoids, and oral antibiotics.
The patient also received pain management strategies. The response to treatment was gradual, with improvement observed after several weeks of therapy. While the condition didn’t fully resolve, the severity of the pustules significantly decreased, and the patient experienced a substantial reduction in pain. Key lessons learned from this case underscore the importance of recognizing the spectrum of acne severity and the need for a multidisciplinary approach to treatment.
Early diagnosis and aggressive management are crucial to minimizing long-term scarring and improving patient quality of life.
Illustration of Acne Conglobata
Imagine a large, inflamed area on the back or chest. Numerous deep, interconnected pustules are visible, varying in size. The surrounding skin is erythematous (reddened) and edematous (swollen). The skin shows significant scarring in the affected areas, a result of the deep inflammation and infection. The image would also depict the varying sizes and depths of the pustules, some appearing as small, inflamed papules or nodules in early stages, and others as large, deep pustules with visible pus.
This illustrates the characteristic appearance of acne conglobata, highlighting the interconnected and extensive nature of the lesions.
Illustration of Different Pustular Rash Types
| Pustular Rash Type | Characteristic Appearance |
|---|---|
| Acne Vulgaris | Small, superficial pustules often associated with comedones (blackheads and whiteheads) on the face, chest, and back. The surrounding skin may be erythematous. |
| Fungal Infections (e.g., Candidiasis) | Clusters of small, superficial pustules, often with satellite lesions (smaller pustules around larger ones), and may have an erythematous base. The skin may appear moist or macerated in certain areas. |
| Pyoderma Gangrenosum | Deep-seated, painful, necrotic pustules often with undermined borders and surrounding erythema. These ulcers can progress rapidly and can be quite extensive. |
| Acute Generalized Exanthematous Pustulosis (AGEP) | Numerous small, superficial, non-follicular pustules distributed diffusely over the body. The pustules appear on an erythematous background, often within a few hours or days of exposure to a medication or infection. |
These illustrations depict the characteristic appearance of various pustular rash types, emphasizing the importance of distinguishing between different presentations. Accurate diagnosis requires careful consideration of the patient’s history, the location and distribution of the lesions, and the associated symptoms.
Epilogue
In conclusion, pustular rash types treatment necessitates a multifaceted approach that considers the unique characteristics of each condition. From understanding the underlying mechanisms to implementing tailored treatment strategies and emphasizing patient education, this guide provides a comprehensive resource for navigating the complexities of pustular rashes. Remember, proper diagnosis and consistent treatment are essential for managing these conditions effectively and minimizing potential complications.










