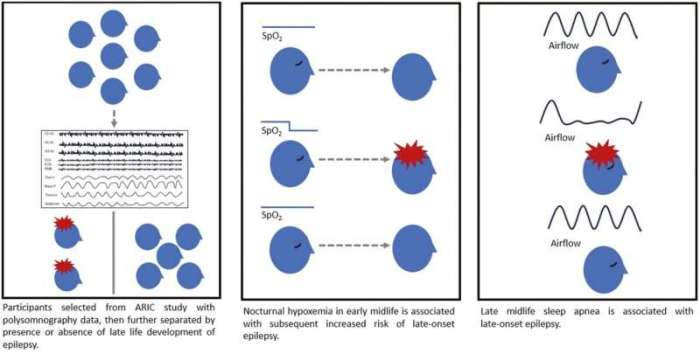
Sleep apnea and oxygen desaturation are closely linked conditions that can significantly impact your health. This in-depth exploration delves into the physiological mechanisms behind sleep apnea, defining oxygen desaturation and highlighting their intricate relationship. We’ll also examine different types of sleep apnea and their effects on oxygen levels, setting the stage for a comprehensive understanding.
From understanding the symptoms and diagnosis methods to exploring the long-term consequences of untreated sleep apnea and oxygen desaturation, this discussion provides a thorough overview. We’ll analyze the impact on cardiovascular health and the connection to other medical conditions. Furthermore, we’ll explore various treatment options, including the critical role of CPAP therapy, along with lifestyle factors and preventative measures.
Introduction to Sleep Apnea and Oxygen Desaturation
Sleep apnea is a common sleep disorder characterized by pauses in breathing during sleep. These pauses can last for several seconds to minutes, disrupting the normal flow of oxygen to the body. The consequences of these interruptions can be significant, impacting not only sleep quality but also overall health. Understanding the physiological mechanisms behind sleep apnea and the resulting oxygen desaturation is crucial for diagnosis and effective treatment.The physiological mechanisms of sleep apnea are multifaceted.
The most common type, obstructive sleep apnea, occurs when the muscles in the throat relax during sleep, causing the airway to narrow or collapse. This blockage prevents air from flowing freely, leading to the characteristic pauses in breathing. Central sleep apnea, a less common type, involves a failure of the brain to signal the muscles responsible for breathing.
Both types of apnea can result in oxygen desaturation, a critical drop in the level of oxygen in the blood.
Defining Oxygen Desaturation
Oxygen desaturation is a reduction in the amount of oxygen carried by the blood. Normal blood oxygen saturation levels are typically between 95% and 100%. When oxygen saturation falls below this range, it indicates a potential problem with the body’s ability to efficiently deliver oxygen to tissues. This decrease can occur due to various factors, but sleep apnea is a significant contributor.
Relationship Between Sleep Apnea and Oxygen Desaturation
Sleep apnea directly impacts oxygen saturation levels. During apneic episodes, oxygen delivery to the body is interrupted. As a result, the blood’s oxygen concentration decreases, leading to oxygen desaturation. This repeated cycle of oxygen deprivation during sleep can have profound consequences on various bodily functions. The severity of desaturation correlates with the frequency and duration of apneic episodes.
For example, a person experiencing frequent and prolonged apneic events will likely exhibit more significant and frequent drops in oxygen saturation.
Sleep apnea and oxygen desaturation can be seriously disruptive, impacting various bodily functions. While the exact causes of triple negative breast cancer, like some other health issues , are still being researched, the link to overall health and wellness is clear. Ultimately, prioritizing sleep and addressing potential oxygen desaturation issues is crucial for maintaining a healthy lifestyle.
Types of Sleep Apnea and Their Impact on Oxygen Levels
Understanding the different types of sleep apnea and their respective impacts on oxygen levels is essential for appropriate diagnosis and treatment. Different types of sleep apnea affect the body in varying ways.
| Type of Sleep Apnea | Mechanism | Impact on Oxygen Levels |
|---|---|---|
| Obstructive Sleep Apnea (OSA) | Airflow blockage due to relaxation of throat muscles | Significant and frequent oxygen desaturation events. Oxygen levels can fluctuate greatly. |
| Central Sleep Apnea (CSA) | Brain’s failure to signal breathing muscles | Oxygen desaturation episodes can occur, often less frequent and potentially less severe compared to OSA, but can still cause significant disruption. |
| Mixed Sleep Apnea | Combination of obstructive and central sleep apnea | Oxygen desaturation events exhibit characteristics of both OSA and CSA, demonstrating a more complex and variable pattern. |
Symptoms and Diagnosis
Unmasking sleep apnea and oxygen desaturation often requires a careful evaluation of symptoms and employing appropriate diagnostic tools. Recognizing the signs and understanding the diagnostic process are crucial steps in obtaining an accurate diagnosis and developing an effective treatment plan. This section delves into the common symptoms, diagnostic methods, and criteria used to identify these conditions.Identifying the subtle indicators of sleep apnea and oxygen desaturation is vital for prompt intervention.
Many individuals experience these issues without realizing their significance, highlighting the importance of proactive health assessments. A comprehensive understanding of both the symptoms and the diagnostic processes is paramount for early intervention and effective management.
Common Symptoms of Sleep Apnea and Oxygen Desaturation
Symptoms associated with sleep apnea and oxygen desaturation can vary in intensity and presentation. These conditions can manifest in both subtle and pronounced ways, making self-diagnosis challenging. Recognizing the potential symptoms can encourage individuals to seek professional medical attention.
- Loud snoring: A persistent, often loud snoring sound during sleep can be a significant indicator of sleep apnea. This occurs due to the narrowing or blockage of the airway during sleep.
- Excessive daytime sleepiness: Feeling unusually tired or sleepy during the day, even after a full night’s sleep, is another common symptom. This is often a result of disrupted sleep patterns and the reduced oxygen supply during sleep.
- Morning headaches: Waking up with a headache, particularly in the morning, can sometimes be a sign of sleep apnea. This is linked to the fluctuations in blood oxygen levels throughout the night.
- Difficulty concentrating: Reduced cognitive function and difficulty concentrating during the day are also common symptoms. The lack of adequate oxygen during sleep can impact brain function.
- Dry mouth: Waking up with a dry mouth can be an indicator of sleep apnea. This is attributed to the pauses in breathing during sleep.
Diagnostic Methods for Sleep Apnea
Several methods are employed to diagnose sleep apnea and assess oxygen desaturation. The choice of method depends on the specific clinical presentation and suspected severity.
- Polysomnography (PSG): This is the gold standard diagnostic test for sleep apnea. It involves monitoring various physiological parameters during sleep, including brain waves, eye movements, breathing patterns, oxygen saturation, and heart rate. During the test, sensors are placed on the patient’s head, face, and chest. The test is conducted overnight in a sleep laboratory or specialized clinic.
This comprehensive assessment provides a detailed picture of the sleep-related breathing issues and oxygen desaturation patterns.
- Home Sleep Studies (HST): If a PSG is not immediately feasible or necessary, a home sleep study can be a viable alternative. This test uses portable equipment to monitor the same physiological parameters as a PSG, but it is performed in the comfort of the patient’s home. Home sleep studies are suitable for patients who are not suitable candidates for a sleep study in a lab.
Results from HSTs are often reviewed and interpreted by a sleep specialist.
- Physical Examination: A physical examination can reveal clues suggestive of sleep apnea. A doctor may evaluate the patient’s neck circumference, presence of obesity, and other relevant physical factors that are associated with the condition. This provides initial information to aid in further diagnostic steps.
Diagnostic Criteria for Sleep Apnea
Specific criteria are used to establish a diagnosis of sleep apnea. These criteria typically involve the number of apnea and hypopnea events per hour of sleep, as well as the degree of oxygen desaturation experienced during sleep.
A diagnosis of sleep apnea is generally established based on the Apnea-Hypopnea Index (AHI).
Comparison of Diagnostic Tests
| Diagnostic Test | Description | Advantages | Disadvantages |
|---|---|---|---|
| Polysomnography (PSG) | Comprehensive overnight sleep study | Gold standard, detailed data | Requires overnight stay in a sleep lab, more expensive |
| Home Sleep Study (HST) | Portable overnight sleep study | More convenient, less expensive | May not capture all nuances of sleep apnea, potentially less accurate |
| Physical Examination | Initial evaluation of patient | Simple, non-invasive | Limited in providing definitive diagnosis |
Consequences and Complications
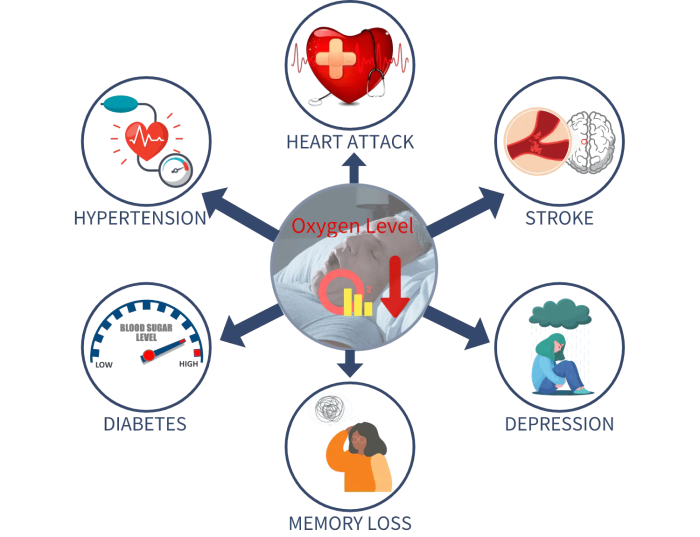
Untreated sleep apnea and oxygen desaturation can have serious, long-lasting consequences on various aspects of health. These conditions disrupt the body’s natural restorative processes during sleep, leading to a cascade of potential problems. Understanding these consequences is crucial for proactive management and improved overall well-being.The chronic nature of these issues, often experienced over many years, can contribute to a range of complications.
The persistent lack of adequate oxygen during sleep and the disruption of normal sleep cycles can place undue stress on vital organs, leading to significant health concerns. Recognizing these connections is essential for effective preventative measures.
Cardiovascular Impacts
Sleep apnea and oxygen desaturation significantly impact cardiovascular health. These conditions are strongly linked to an increased risk of hypertension (high blood pressure). The repeated drops in oxygen levels and arousal from sleep can trigger a surge in stress hormones, contributing to elevated blood pressure readings over time. Furthermore, the disrupted sleep patterns can negatively affect the heart’s ability to regulate blood pressure effectively.
This can increase the risk of developing heart failure, a condition where the heart struggles to pump enough blood to meet the body’s needs. Studies have shown a correlation between untreated sleep apnea and an increased risk of stroke and coronary artery disease.
Connection to Other Medical Conditions
Sleep apnea and oxygen desaturation are not isolated problems. They are linked to a variety of other medical conditions, often exacerbating existing issues or contributing to the development of new ones. For example, these sleep disorders are frequently associated with type 2 diabetes, as the body’s ability to regulate blood sugar can be negatively affected by chronic sleep deprivation and oxygen deprivation.
The persistent inflammation caused by sleep apnea can also contribute to chronic inflammation throughout the body, increasing the risk of developing conditions like rheumatoid arthritis. The disruption of normal sleep cycles can affect the body’s ability to repair and regenerate, potentially impacting overall health and well-being.
Potential Complications
A variety of complications can arise from untreated sleep apnea and oxygen desaturation. The following table Artikels some of the potential consequences.
| Condition | Description |
|---|---|
| Cardiovascular Disease | Increased risk of high blood pressure, heart failure, stroke, and coronary artery disease. |
| Metabolic Disorders | Increased risk of type 2 diabetes, insulin resistance, and impaired glucose tolerance. |
| Neurological Problems | Increased risk of cognitive impairment, depression, anxiety, and mood disorders. Concentration problems and memory issues can also arise. |
| Sleep Disorders | Chronic fatigue, daytime sleepiness, and difficulty concentrating can severely affect daily life. |
| Respiratory Issues | Increased risk of respiratory infections, such as pneumonia, and worsening of existing respiratory conditions. |
| Gastrointestinal Problems | Possible link to gastroesophageal reflux disease (GERD). |
Treatment Options
Managing sleep apnea and oxygen desaturation requires a multifaceted approach tailored to the individual’s specific needs and severity of the condition. Treatment options range from lifestyle modifications to advanced medical interventions. Understanding the various choices and their potential benefits and drawbacks is crucial for making informed decisions.
CPAP Therapy
Continuous Positive Airway Pressure (CPAP) therapy is the most common and often the first-line treatment for obstructive sleep apnea. A CPAP machine delivers a continuous flow of air pressure through a mask worn during sleep. This pressure helps keep the airways open, preventing the collapse that leads to apnea episodes.
- CPAP therapy is highly effective in reducing apnea events and improving oxygen saturation levels during sleep. Studies have shown significant improvements in sleep quality and daytime functioning for many patients.
- The consistent positive pressure helps maintain a patent airway, preventing the recurrent collapses that cause apneas and hypopneas. This leads to a more restful night’s sleep and improved oxygenation.
Lifestyle Modifications
Several lifestyle changes can complement or even be the primary treatment for mild sleep apnea cases. These modifications often involve addressing underlying contributing factors.
- Weight loss is often a crucial component of managing sleep apnea. Excess weight can put pressure on the airway, making it more prone to collapse. A 10% reduction in body weight can often significantly improve symptoms.
- Avoiding alcohol and sedatives before bed can also help alleviate sleep apnea symptoms. These substances relax the muscles in the throat and can worsen the tendency towards airway blockage.
- Sleeping on your side instead of your back can reduce the likelihood of airway obstruction. This simple change can significantly impact the severity of sleep apnea episodes.
Oral Appliances
Oral appliances are custom-fitted devices worn in the mouth during sleep. They reposition the jaw and tongue, preventing the airway from collapsing. They are often a good option for individuals who cannot tolerate CPAP therapy.
- Oral appliances are a non-invasive alternative to CPAP, and they can be particularly beneficial for individuals who have difficulty tolerating a CPAP mask.
- They are effective in improving airway patency and reducing apnea events. However, their effectiveness may vary depending on the severity of the sleep apnea and the specific characteristics of the patient’s airway.
Surgery
Surgical interventions are reserved for cases where other treatments are ineffective or inappropriate. These procedures aim to correct structural abnormalities in the airway.
Sleep apnea and oxygen desaturation can be tricky, impacting overall health. While focusing on a balanced diet is crucial, exploring alternatives like almond milk can be beneficial. A great resource for understanding if almond milk is a healthy addition to your diet is this article on is almond milk good for you. Ultimately, maintaining healthy sleep patterns and oxygen levels is key to combating sleep apnea and its related health issues.
- Uvulopalatopharyngoplasty (UPPP) is a surgical procedure that removes or modifies tissues in the back of the throat to widen the airway.
- Other surgical options might include the use of implants or other techniques to enhance the structural support of the airway. These procedures should be considered only after other treatment options have been exhausted.
Role of CPAP in Oxygen Desaturation
CPAP therapy plays a crucial role in managing oxygen desaturation by maintaining a constant pressure within the airway. This pressure counteracts the tendency for the airway to collapse, preventing the recurrent episodes of apnea and hypopnea. Consequently, oxygen levels in the blood are maintained within a healthy range throughout the night.
Summary of Treatment Options
| Treatment Option | Advantages | Disadvantages |
|---|---|---|
| CPAP | Effective in reducing apnea events, improving oxygen saturation, often first-line treatment | Can be uncomfortable for some, requires compliance, potential for mask leaks |
| Lifestyle Modifications | Non-invasive, often low cost, addresses underlying causes | May not be sufficient for severe sleep apnea, requires commitment to changes |
| Oral Appliances | Non-invasive, often well-tolerated alternative to CPAP | May not be effective for all cases, potential for discomfort or jaw pain |
| Surgery | Potentially curative for some structural abnormalities | Invasive, carries risks of complications, usually last resort |
Lifestyle Factors and Prevention
Lifestyle plays a crucial role in managing and preventing sleep apnea and oxygen desaturation. Making conscious choices about diet, exercise, and sleep habits can significantly reduce the risk and severity of these conditions. Adopting healthy lifestyle practices not only improves sleep quality but also contributes to overall health and well-being.Adopting a healthy lifestyle isn’t just about preventing sleep apnea and oxygen desaturation; it’s about improving overall health and well-being.
By prioritizing healthy habits, individuals can reduce their risk of developing these conditions and potentially improve their quality of life.
The Role of Sleep Hygiene, Sleep apnea and oxygen desaturation
Proper sleep hygiene is fundamental in mitigating the risk of sleep apnea and oxygen desaturation. A consistent sleep schedule, a relaxing bedtime routine, and a conducive sleep environment can significantly improve sleep quality. This, in turn, can reduce the likelihood of apnea episodes and improve oxygen saturation levels during sleep.
- Consistent Sleep Schedule: Establishing a regular sleep-wake cycle, even on weekends, helps regulate the body’s natural sleep-wake rhythm. This regularity can improve sleep quality and reduce the occurrence of sleep disturbances, which are often linked to sleep apnea.
- Relaxing Bedtime Routine: A calming bedtime routine, such as taking a warm bath, reading a book, or listening to soothing music, can signal to the body that it’s time to wind down. Avoid screens or stimulating activities close to bedtime, as these can interfere with sleep onset.
- Conducive Sleep Environment: A dark, quiet, and cool bedroom environment promotes better sleep. Minimizing noise and light distractions can enhance sleep quality and reduce the risk of sleep apnea.
Obesity and Sleep Apnea
Obesity is a significant risk factor for sleep apnea and oxygen desaturation. The excess weight and fat tissue, particularly around the neck and upper airway, can obstruct the airway during sleep, leading to reduced airflow and oxygen levels. This is because the extra weight can cause the tissues in the throat and airways to collapse, leading to an obstruction.
Maintaining a Healthy Weight and Regular Exercise
Maintaining a healthy weight and incorporating regular exercise into one’s routine are essential for preventing and managing sleep apnea and oxygen desaturation. Weight loss, even modest amounts, can significantly improve sleep quality and reduce the severity of apnea episodes.
- Healthy Weight Management: Maintaining a healthy body mass index (BMI) is crucial for reducing the risk of sleep apnea. Weight loss, even a small amount, can help improve airflow during sleep and reduce the severity of apnea episodes. Dietary changes, coupled with regular exercise, are crucial for achieving and maintaining a healthy weight.
- Regular Exercise: Regular physical activity is beneficial for overall health and contributes to weight management. Exercise strengthens the muscles involved in breathing, potentially improving airflow during sleep. Physical activity also helps in improving cardiovascular health, which is vital in managing sleep apnea.
Lifestyle Modifications for Reducing Risk
Implementing lifestyle modifications can significantly reduce the risk of sleep apnea and oxygen desaturation. These modifications focus on improving sleep hygiene, managing weight, and promoting overall health.
| Lifestyle Modification | Description |
|---|---|
| Consistent Sleep Schedule | Establish a regular sleep-wake cycle, even on weekends, to regulate the body’s natural sleep-wake rhythm. |
| Relaxing Bedtime Routine | Engage in calming activities before bed, such as taking a warm bath or reading a book, to signal the body to wind down. |
| Healthy Diet | Consume a balanced diet rich in fruits, vegetables, and whole grains, and limit processed foods, sugary drinks, and unhealthy fats. |
| Regular Exercise | Engage in regular physical activity, such as brisk walking, jogging, or swimming, to maintain a healthy weight and improve cardiovascular health. |
| Weight Management | Maintain a healthy weight through a combination of a balanced diet and regular exercise. |
| Avoid Alcohol and Smoking | Reduce or eliminate alcohol and smoking as these habits can worsen sleep apnea and oxygen desaturation. |
Monitoring and Management
Staying on top of sleep apnea and oxygen desaturation requires a proactive approach. Continuous monitoring and meticulous management are crucial for effectively controlling symptoms and preventing complications. This involves understanding the various methods available and actively participating in your care.Effective management of sleep apnea and oxygen desaturation relies on consistent monitoring of oxygen levels during sleep and implementing appropriate treatment strategies.
Understanding how to interpret the data and make informed decisions with your healthcare provider is vital for optimizing your well-being.
Methods for Continuous Monitoring of Oxygen Saturation During Sleep
Continuous monitoring of oxygen saturation during sleep is achieved through a variety of methods, primarily using devices worn on the body. These devices continuously measure the amount of oxygen in your blood. Common methods include pulse oximeters, which are clipped onto a finger, and more comprehensive sleep studies.
Hey everyone! So, I’ve been researching sleep apnea and oxygen desaturation lately, and it’s fascinating how much our bodies can struggle when we’re not getting enough restful sleep. Speaking of struggles, have you ever wondered why you might get diarrhea during your period? There are a lot of theories out there, and you can find some great info on this topic at why do i have diarrhea on my period.
It seems like hormonal fluctuations can play a big role, and it’s all connected back to the body’s complex responses to the changing environment during menstruation. Back to sleep apnea, understanding these sorts of bodily reactions could offer a better understanding of the effects of oxygen desaturation on the whole system.
- Pulse Oximeters: These small, non-invasive devices clip onto a finger or toe and measure oxygen saturation (SpO2) in the blood. They provide a real-time reading of your blood oxygen levels. Pulse oximeters are commonly used for home monitoring and can be invaluable for detecting episodes of desaturation, even in their early stages.
- Sleep Studies (Polysomnography): These studies are performed in a sleep lab or at home and involve multiple measurements. They track various physiological parameters, including oxygen saturation, heart rate, breathing patterns, and brain waves. This comprehensive approach provides a detailed record of your sleep and identifies specific patterns of sleep apnea and oxygen desaturation. A sleep study provides crucial data for diagnosis and treatment tailoring.
Procedures for Managing Sleep Apnea and Oxygen Desaturation
Managing sleep apnea and oxygen desaturation involves a multifaceted approach, often combining several strategies. The precise approach is tailored to the individual’s specific needs and severity of the condition.
- CPAP (Continuous Positive Airway Pressure) Therapy: A common treatment for sleep apnea, CPAP involves wearing a mask that delivers a continuous flow of air pressure to keep the airways open during sleep. This helps prevent episodes of apnea and improves oxygen saturation levels. Proper mask fitting and pressure adjustments are essential for optimal effectiveness.
- BiPAP (Bilevel Positive Airway Pressure) Therapy: Similar to CPAP, but BiPAP delivers two different air pressures – one for inhalation and one for exhalation. This therapy is sometimes preferred for individuals who find CPAP uncomfortable or less effective.
- Lifestyle Modifications: This often includes weight loss, avoiding alcohol and sedatives before bed, and adopting better sleep hygiene practices. These lifestyle adjustments can significantly impact sleep apnea severity and oxygen saturation levels.
Tracking Oxygen Saturation Levels at Home
Monitoring oxygen saturation levels at home is a valuable tool for proactive management of sleep apnea and desaturation.
- Using a Pulse Oximeter: Pulse oximeters can be used to track oxygen saturation levels throughout the day or at specific times, such as before bed, after waking up, or after exertion. Record these readings in a logbook or app for analysis and discussion with your healthcare provider. Consistency in your monitoring and reporting will assist your provider in identifying patterns and trends.
Interpreting Oxygen Saturation Data
Interpreting oxygen saturation data requires understanding the context and baseline values. Your doctor will provide a range of acceptable values for your particular situation, and deviation from this range may indicate the need for intervention.
- Normal Values: Normal oxygen saturation levels (SpO2) generally range between 95% and 100% during wakefulness. Lower readings, particularly during sleep, can be indicative of sleep apnea and oxygen desaturation.
- Variability: Recognize that oxygen saturation levels can fluctuate throughout the day and night. Understanding these fluctuations helps in identifying patterns and areas for improvement.
- Consistency: Consistency in monitoring and recording your oxygen saturation levels is essential for understanding trends and patterns. This information is crucial in informing treatment decisions and optimizing management strategies.
Summary Table: Monitoring and Managing Oxygen Saturation Levels
| Method | Description | Example |
|---|---|---|
| Pulse Oximeter | Non-invasive device measuring SpO2 | Track levels throughout the day, especially at night. |
| Sleep Study | Comprehensive sleep evaluation | Identify patterns of apnea and desaturation. |
| CPAP/BiPAP | Positive airway pressure therapy | Improve airway pressure and oxygen saturation. |
| Lifestyle Changes | Weight loss, sleep hygiene | Reduce apnea severity and improve oxygen saturation. |
Illustrative Case Studies
Understanding sleep apnea and oxygen desaturation requires looking at how these conditions affect individuals. Real-world examples highlight the diverse ways these issues manifest and how different management approaches play out. This section presents case studies demonstrating the impact of sleep apnea and oxygen desaturation on health, successful management strategies, and factors influencing individual responses to treatment.
Impact on Individual Health
Sleep apnea and oxygen desaturation can significantly impact various aspects of a person’s life. They can lead to daytime fatigue, difficulty concentrating, and an increased risk of accidents. These individuals often report feeling irritable, depressed, or anxious. Furthermore, untreated sleep apnea can contribute to high blood pressure, heart disease, stroke, and type 2 diabetes. The severity of these impacts varies greatly from person to person, depending on factors such as the duration and severity of the sleep disorder, pre-existing health conditions, and individual response to treatment.
Successful Management Strategies
Effective management strategies for sleep apnea and oxygen desaturation involve a multi-faceted approach. These strategies often include a combination of lifestyle changes, medical interventions, and ongoing monitoring. Successful management relies heavily on patient adherence to prescribed treatments and lifestyle modifications. A key component is educating patients about the importance of consistent adherence to their treatment plan.
Factors Contributing to Individual Responses to Treatment
Several factors influence how individuals respond to treatment for sleep apnea and oxygen desaturation. Age, overall health, pre-existing conditions, and the severity of the sleep disorder all play a role. The patient’s motivation and willingness to make lifestyle changes significantly impact the effectiveness of the treatment. Additionally, the quality of the support system, including family, friends, and healthcare providers, plays a crucial part in the patient’s ability to successfully manage the condition.
Long-Term Outcomes of Different Management Approaches
The long-term outcomes of different management approaches for sleep apnea and oxygen desaturation vary based on factors like adherence to treatment plans and individual characteristics. Consistent use of CPAP (Continuous Positive Airway Pressure) therapy, for example, can lead to significant improvements in sleep quality, daytime function, and overall health. In contrast, patients who struggle with adherence to therapy may experience more persistent symptoms and potentially more serious health complications.
Long-term monitoring and adjustments to the treatment plan are often necessary to ensure optimal outcomes.
Case Study Examples
| Case Study | Patient Characteristics | Management Approach | Long-Term Outcomes |
|---|---|---|---|
| Case 1 | 45-year-old male, obese, with a history of hypertension | CPAP therapy, weight loss program, dietary modifications | Significant improvement in sleep quality, reduced daytime fatigue, and controlled blood pressure. |
| Case 2 | 62-year-old female, with pre-existing heart disease, mild sleep apnea | CPAP therapy, lifestyle adjustments, regular follow-up appointments | Improved sleep quality and reduced episodes of oxygen desaturation. Continued monitoring to address potential cardiac complications. |
| Case 3 | 28-year-old male, active lifestyle, moderate sleep apnea | Lifestyle modifications (regular exercise, healthy diet), oral appliance therapy | Improved sleep quality and daytime alertness. Continued need for monitoring and follow-up. |
Final Thoughts: Sleep Apnea And Oxygen Desaturation
In conclusion, sleep apnea and oxygen desaturation present a complex interplay of physiological and lifestyle factors. Understanding the symptoms, diagnostic processes, and potential complications is crucial for effective management. Treatment options range from lifestyle modifications to advanced therapies like CPAP, underscoring the importance of early diagnosis and consistent monitoring. Ultimately, proactive measures and a holistic approach can significantly improve outcomes and quality of life for those affected by these conditions.










