Symptoms of sleep paralysis can be terrifying. Imagine waking up, unable to move, with a heavy feeling on your chest, accompanied by vivid hallucinations. This unsettling experience, known as sleep paralysis, affects millions worldwide, and understanding its symptoms is key to managing and coping with it. This exploration delves into the various aspects of sleep paralysis, from its causes to its treatment, providing a comprehensive overview of this often misunderstood phenomenon.
This article will discuss the physical sensations, emotional responses, and sensory experiences associated with sleep paralysis, shedding light on the neurological mechanisms that might be involved. We’ll also explore how sleep disorders, stress, and certain medications might contribute to sleep paralysis. Furthermore, it will cover diagnosis and assessment methods, alongside various management and treatment strategies, to help you navigate this often-frightening condition.
Introduction to Sleep Paralysis: Symptoms Of Sleep Paralysis
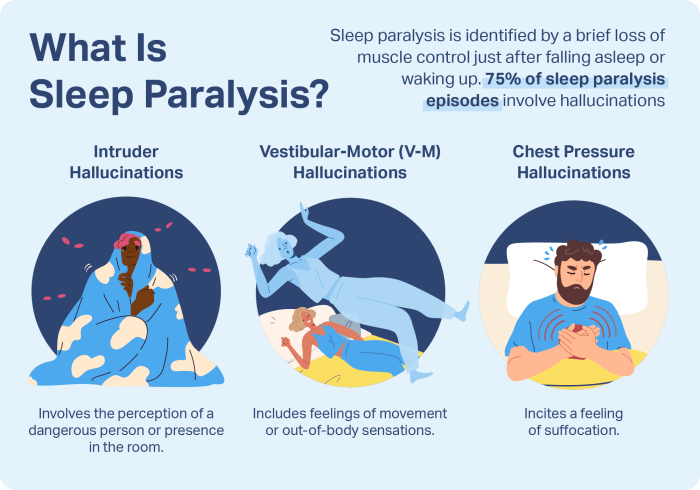
Sleep paralysis is a temporary inability to move or speak that occurs when transitioning between sleep and wakefulness. This often happens at the onset or end of sleep, leaving individuals feeling trapped and vulnerable. It’s a common experience, though often frightening, and typically resolves on its own.Sleep paralysis is characterized by a range of sensations, often accompanied by hallucinations.
These experiences can vary from feeling a presence in the room to feeling like something is suffocating the individual. The feeling of being unable to move or speak, coupled with these sensory experiences, can contribute to significant anxiety and distress.
Prevalence of Sleep Paralysis
Sleep paralysis affects a substantial portion of the population, though the exact prevalence can vary based on the study methodology. Estimates suggest that a significant percentage of people will experience it at least once in their lives. Furthermore, certain demographic factors might increase susceptibility.
Potential Triggers for Sleep Paralysis
Several factors can increase the likelihood of experiencing sleep paralysis. These include sleep deprivation, irregular sleep schedules, stress, anxiety, and certain medical conditions. Poor sleep hygiene practices, like inconsistent sleep times and environments, are also implicated in triggering sleep paralysis.
Characteristics of Sleep Paralysis
Sleep paralysis typically involves an inability to move or speak while transitioning between sleep and wakefulness. Individuals experiencing sleep paralysis may also report hallucinations, such as the sensation of a presence or a feeling of being suffocated. The duration of an episode can vary, typically lasting from a few seconds to a few minutes.
Experiencing sleep paralysis can be a truly unsettling experience, marked by the feeling of being trapped and unable to move. While it’s often just a temporary disruption, it can be incredibly frightening. Interestingly, there are some parallels between the temporary inability to move during sleep paralysis and the permanent vision loss some babies and children experience due to congenital cataracts.
For more information on congenital cataracts vision loss in babies and children, check out this helpful resource: congenital cataracts vision loss babies children. Regardless of the cause, understanding these experiences can help us better cope with them and seek appropriate medical attention if needed.
Types of Sleep Paralysis (If Applicable)
While there are not distinct “types” of sleep paralysis in a clinical sense, there are different classifications based on the accompanying experiences. However, these are more descriptive rather than distinct types.
| Classification | Description |
|---|---|
| Typical Sleep Paralysis | The most common type, characterized by the inability to move or speak, often accompanied by hallucinations. |
| Sleep Paralysis with Hallucinations | Similar to typical sleep paralysis but involves vivid and sometimes frightening hallucinations, which can include feelings of being watched or attacked. |
| Sleep Paralysis with a Sense of Presence | Individuals experiencing this type describe a feeling of a presence in the room, often accompanied by feelings of dread or fear. |
Symptoms and Experiences
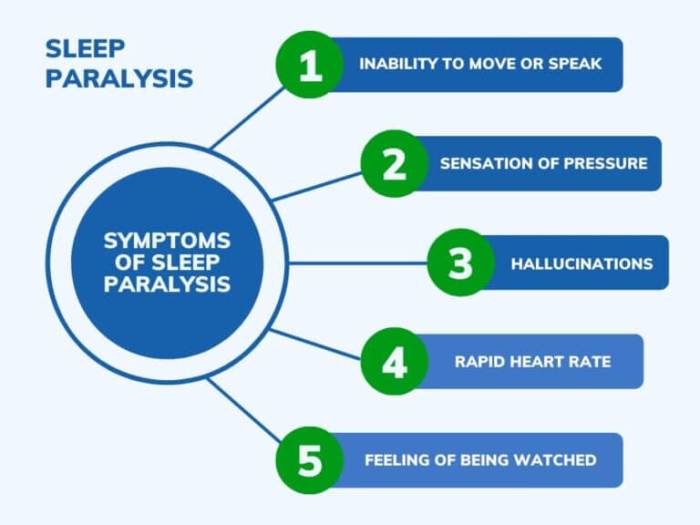
Sleep paralysis, a perplexing and often terrifying experience, is characterized by a range of physical, emotional, and sensory symptoms. Understanding these symptoms is crucial for recognizing and managing this condition, as well as for distinguishing it from other potential medical issues. While the precise mechanisms are still being investigated, the experiences reported are remarkably consistent across individuals.Sleep paralysis is not simply a frightening feeling; it’s a complex interplay of physiological and psychological responses that can manifest in a variety of ways.
The combination of a temporary inability to move while fully awake and often accompanying hallucinations creates a powerful and unsettling experience.
Physical Sensations
The most common physical sensation associated with sleep paralysis is the inability to move, speak, or react despite being fully conscious. This feeling of being trapped is often accompanied by a range of other physical sensations. Individuals might experience pressure on the chest, difficulty breathing, or a sense of suffocation. These physical sensations are often amplified by the accompanying emotional responses.
- Immobility: The inability to move voluntarily, despite being fully aware, is a core symptom of sleep paralysis. This can range from a slight difficulty in initiating movement to a complete inability to move any part of the body.
- Pressure or Pain: Some individuals report feeling pressure or pain, particularly in the chest area, often accompanied by feelings of suffocation or difficulty breathing. This is likely related to the heightened anxiety and stress response.
- Sensory Disturbances: While not strictly physical, the experience of pressure and pain can be intense, leading to sensations similar to those found in physical symptoms. The combination of physical immobility and sensations intensifies the emotional response.
Emotional Responses
Sleep paralysis frequently triggers intense emotional responses, ranging from fear and anxiety to panic and terror. The sudden onset of immobility, coupled with the often vivid hallucinations, can lead to a significant emotional distress response.
Experiencing sleep paralysis can be a truly unsettling experience, marked by the inability to move or speak while falling asleep or waking up. While the exact causes remain somewhat mysterious, some studies suggest a connection between sleep disorders and other health concerns. For example, issues like obesity can significantly impact bone health, increasing fracture risk, which is something to be aware of if you’re dealing with sleep paralysis or other related symptoms.
Learning more about the potential links between these conditions, such as exploring obesity and fracture risk , might help in understanding the bigger picture of your overall health. Ultimately, sleep paralysis itself warrants further investigation and understanding.
- Fear and Anxiety: The inability to move and the feeling of being trapped can be profoundly frightening. This fear is often amplified by the accompanying sensory experiences, such as hallucinations, which can seem very real in the moment.
- Panic and Terror: In some cases, sleep paralysis can escalate to a state of panic and terror. The inability to escape or control the situation can be overwhelming and cause significant distress.
Sensory Experiences
Sensory hallucinations, including auditory and visual experiences, are common during sleep paralysis. These hallucinations are often vivid and frightening, contributing to the overall sense of unease.
- Auditory Hallucinations: Individuals may hear noises such as whispers, footsteps, or other sounds that seem to originate from outside their body, adding to the sense of being watched or threatened. The intensity and clarity of these auditory hallucinations can vary greatly.
- Visual Hallucinations: Similarly, visual hallucinations can involve seeing shadowy figures, monsters, or other frightening images. These visual experiences can be highly realistic and unsettling, contributing to the feeling of being overwhelmed and out of control.
Fear, Panic, and Anxiety
The combination of physical sensations, emotional responses, and sensory experiences often results in feelings of fear, panic, or anxiety. This can lead to a heightened stress response and further complicate the experience.
- Escalation of Fear: The fear associated with sleep paralysis can escalate quickly, making the experience intensely distressing. The combination of immobility and sensory experiences can contribute to the feeling of being in immediate danger.
Potential Symptoms and Intensities
| Symptom | Intensity (Low – High) |
|---|---|
| Immobility | Low – High |
| Pressure/Pain | Low – High |
| Auditory Hallucinations | Low – High |
| Visual Hallucinations | Low – High |
| Fear/Anxiety | Low – High |
| Panic/Terror | Low – High |
Underlying Causes and Risk Factors
Sleep paralysis, that terrifying feeling of being trapped between wakefulness and sleep, isn’t just a spooky experience; it’s a real phenomenon with potential underlying causes. Understanding these factors can help individuals better manage and even potentially prevent episodes. The exact mechanisms behind sleep paralysis are still being researched, but a confluence of factors is likely at play.Sleep paralysis is often linked to disruptions in the normal sleep cycle.
Our brains and bodies experience a complex interplay during sleep, and when this cycle is disrupted, unusual experiences like sleep paralysis can arise. Many factors can contribute to these disruptions, ranging from stress and lifestyle to underlying medical conditions.
Neurological Mechanisms, Symptoms of sleep paralysis
Sleep paralysis is believed to occur when the brain’s natural processes for controlling muscle movement during REM (Rapid Eye Movement) sleep are disrupted. Normally, during REM sleep, the brain signals the body to temporarily paralyze muscles to prevent us from acting out our dreams. In sleep paralysis, this signal may be delayed or incomplete, leaving the individual conscious but unable to move.
The brain is still processing the dream state, while the body is unable to respond to conscious commands. This can lead to feelings of fear, helplessness, and the feeling of an external presence.
Role of Sleep Disorders
Sleep disorders, such as insomnia and sleep apnea, significantly impact sleep quality and quantity. Insomnia, characterized by difficulty falling asleep or staying asleep, can disrupt the delicate balance of the sleep cycle, increasing the likelihood of sleep paralysis episodes. Sleep apnea, a disorder where breathing repeatedly stops and starts during sleep, can also disrupt sleep architecture, leading to fragmented sleep and potential sleep paralysis occurrences.
These disruptions can lead to a greater susceptibility to experiencing sleep paralysis.
Stress and Anxiety
High levels of stress and anxiety are strongly associated with an increased risk of sleep paralysis. Stress can disrupt the delicate balance of the sleep cycle, making it more likely that the muscle-paralysis mechanism during REM sleep will malfunction. Anxiety can exacerbate these disruptions, contributing to heightened emotional responses during sleep paralysis episodes. Furthermore, stress can lead to poor sleep quality, which in turn can increase the likelihood of experiencing this phenomenon.
Medications and Substances
Certain medications and substances can interfere with the sleep cycle, potentially triggering or exacerbating sleep paralysis. Stimulants, depressants, and some medications for various conditions, including allergies, asthma, and even some antidepressants, may impact the natural processes involved in sleep, increasing the risk of sleep paralysis. It is important to discuss the potential effects of any medication with a healthcare professional.
Comparison of Risk Factors Across Age Groups
| Age Group | Potential Risk Factors | Explanation |
|---|---|---|
| Children (ages 0-12) | Rapid growth spurts, developmental sleep disorders, and stress from school and home life. | Sleep paralysis in children may be linked to changes in their developing sleep patterns. Stressful life events can also play a role. |
| Adolescents (ages 13-19) | Hormonal changes, irregular sleep schedules, stress related to academics and social life, and increased substance use. | Significant hormonal fluctuations during adolescence can disrupt sleep cycles. Increased pressure from academics and social life contribute to higher stress levels, potentially leading to more sleep paralysis episodes. |
| Adults (ages 20-64) | Stressful life events, shift work, sleep disorders, and the use of certain medications. | Adults are often dealing with high-pressure jobs, family responsibilities, and other stressors. Sleep disorders and medication use can significantly affect sleep quality. |
| Seniors (ages 65+) | Underlying medical conditions, medications, and changes in sleep patterns associated with aging. | Seniors may experience a variety of health conditions that can impact sleep. Medications for these conditions are a potential factor. |
Diagnosis and Assessment
Figuring out what’s causing those terrifying sleep paralysis episodes is crucial for effective treatment. This involves a multi-faceted approach, combining patient history, physical examination, and specialized sleep studies. The diagnostic process aims to differentiate sleep paralysis from other similar conditions and pinpoint potential underlying causes.A thorough understanding of the symptoms, frequency, and triggers of sleep paralysis is essential for an accurate diagnosis.
This understanding allows healthcare professionals to develop a tailored treatment plan.
Common Assessment Methods
Gathering a detailed history from the patient is a fundamental part of the assessment. This includes questions about sleep habits, lifestyle factors, stress levels, and any pre-existing medical conditions. Information about the specific symptoms experienced during sleep paralysis episodes, such as hallucinations or the sensation of being trapped, is also vital. A physical examination is performed to rule out any other medical conditions that might be contributing to the symptoms.
Role of Sleep Studies
Polysomnography, or a sleep study, is a crucial tool in evaluating sleep paralysis. It involves monitoring various physiological parameters during sleep, such as brain waves, eye movements, heart rate, and breathing patterns. This comprehensive recording provides valuable insights into the patient’s sleep architecture, identifying any sleep disorders that might be linked to the sleep paralysis episodes. The sleep study helps to rule out other sleep disorders like sleep apnea, narcolepsy, or REM sleep behavior disorder, which can sometimes mimic or be associated with sleep paralysis.
Differentiating Sleep Paralysis from Similar Conditions
Distinguishing sleep paralysis from other conditions is vital. Conditions like panic attacks, anxiety disorders, or even neurological disorders can sometimes exhibit similar symptoms. A careful analysis of the patient’s history, symptoms, and sleep study results is crucial to differentiate sleep paralysis from these other conditions. For example, while panic attacks can involve similar feelings of fear and a sense of impending doom, the specific sensory experiences associated with sleep paralysis, such as hallucinations and a feeling of being unable to move, are unique.
Diagnostic Process Stages
The diagnostic process for sleep paralysis typically involves several key stages:
- Initial Consultation: The process begins with a comprehensive consultation to gather detailed information about the patient’s symptoms, medical history, and lifestyle. This initial interview aims to understand the nature and frequency of sleep paralysis episodes.
- Physical Examination: A physical examination helps to rule out any underlying medical conditions that might be contributing to the sleep paralysis symptoms.
- Sleep History Assessment: A detailed sleep history is crucial, covering sleep patterns, habits, and any pre-existing sleep disorders. The patient’s sleep diary can provide valuable insights.
- Sleep Study (Polysomnography): A sleep study is performed to analyze sleep stages and identify any sleep disorders that might be linked to the sleep paralysis. This allows a comprehensive assessment of sleep patterns.
- Diagnostic Evaluation: The gathered data from the initial consultation, physical examination, sleep history, and sleep study is analyzed to determine if the symptoms are consistent with sleep paralysis. A comparison to other similar conditions is also performed.
- Differential Diagnosis: The results are compared with other conditions to ensure sleep paralysis is the accurate diagnosis.
- Treatment Plan: Based on the diagnosis, a personalized treatment plan is developed to address the specific needs of the patient. This plan might include lifestyle changes, stress management techniques, or medication, if necessary.
Sleep Study Process Steps
A sleep study, also known as polysomnography, involves a series of steps:
| Step | Description |
|---|---|
| Preparation | The patient is instructed to maintain their normal sleep routine as much as possible to ensure accurate results. They may be asked to avoid certain medications or substances that might affect sleep patterns. |
| Equipment Setup | Various sensors are placed on the patient’s body to monitor different physiological functions. These sensors record brain waves, eye movements, heart rate, breathing, leg movements, and more. |
| Data Collection | The equipment continuously records data throughout the night, providing a comprehensive overview of the patient’s sleep stages. |
| Analysis | A sleep specialist reviews the collected data to identify any sleep disorders or abnormalities. |
| Interpretation | The data is interpreted to identify any patterns or issues, especially those relating to sleep paralysis. |
Management and Treatment Strategies
Managing sleep paralysis involves a multifaceted approach that addresses both the immediate symptoms and the underlying contributing factors. Effective strategies often focus on improving sleep quality, managing stress, and employing relaxation techniques. A holistic approach, combining lifestyle changes with potential therapeutic interventions, is frequently recommended.
Non-Pharmacological Management Methods
Various non-pharmacological methods can help manage sleep paralysis. These methods often prove effective in reducing the frequency and intensity of episodes, and they often form the cornerstone of treatment plans. Adopting healthy sleep habits, stress management techniques, and relaxation practices can significantly contribute to alleviating the discomfort associated with sleep paralysis.
- Relaxation Techniques: Progressive muscle relaxation, deep breathing exercises, and mindfulness meditation can help reduce anxiety and promote a sense of calm, particularly before sleep. By consciously releasing tension in various muscle groups, individuals can achieve a state of physical and mental relaxation, potentially decreasing the likelihood of experiencing sleep paralysis.
- Behavioral Therapies: Cognitive behavioral therapy (CBT) for insomnia can be beneficial for individuals experiencing sleep paralysis, particularly if it’s linked to underlying sleep disorders or anxiety. CBT helps identify and modify negative thought patterns and behaviors that may contribute to sleep disturbances.
- Sleep Hygiene Practices: Maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a conducive sleep environment are crucial. A regular sleep-wake cycle regulates the body’s natural sleep-wake rhythm, potentially minimizing disruptions in sleep and reducing the risk of sleep paralysis episodes.
Relaxation Techniques for Sleep Paralysis
Relaxation techniques can significantly alleviate sleep paralysis symptoms. By reducing anxiety and promoting a state of calm, these techniques can help individuals fall asleep more easily and experience less disruption during sleep. Practicing these techniques regularly can establish a positive feedback loop, decreasing the frequency and severity of episodes.
- Progressive Muscle Relaxation: This technique involves systematically tensing and relaxing different muscle groups in the body. This conscious process can help release physical tension, a common contributor to sleep paralysis.
- Deep Breathing Exercises: Slow, deep breaths can calm the nervous system and reduce feelings of anxiety and panic, which are often associated with sleep paralysis. These exercises can help regulate the body’s physiological responses to stress.
- Mindfulness Meditation: Focusing on the present moment without judgment can help individuals detach from racing thoughts and anxieties, both of which can trigger sleep paralysis episodes. This practice promotes a sense of calm and reduces the reactivity to disruptive sensations during sleep.
Behavioral Therapies for Sleep Paralysis
Behavioral therapies, such as cognitive behavioral therapy for insomnia (CBT-I), can be highly effective in addressing sleep paralysis. CBT-I helps individuals identify and modify negative thought patterns and behaviors that contribute to sleep disturbances. This approach often provides long-term benefits for managing sleep paralysis.
- Cognitive Behavioral Therapy for Insomnia (CBT-I): CBT-I is a structured approach that helps individuals identify and challenge negative thoughts and behaviors that contribute to sleep problems. It can be especially beneficial when sleep paralysis is linked to underlying sleep disorders or anxiety.
Sleep Hygiene and Sleep Paralysis
Maintaining good sleep hygiene is essential for preventing and managing sleep paralysis. A consistent sleep schedule, a relaxing bedtime routine, and a conducive sleep environment can significantly improve sleep quality. Creating a regular sleep-wake cycle can help regulate the body’s natural sleep-wake rhythm, potentially minimizing disruptions during sleep and reducing sleep paralysis episodes.
- Consistent Sleep Schedule: Going to bed and waking up around the same time each day, even on weekends, helps regulate the body’s natural sleep-wake cycle.
- Relaxing Bedtime Routine: Establishing a calming bedtime routine, such as reading, taking a warm bath, or listening to relaxing music, can signal to the body that it’s time to sleep.
- Creating a Conducive Sleep Environment: A dark, quiet, and cool bedroom can promote better sleep quality. Minimizing distractions and creating a comfortable sleep environment can reduce the likelihood of sleep paralysis episodes.
Summary of Management Strategies
| Management Strategy | Potential Effectiveness |
|---|---|
| Relaxation techniques (e.g., progressive muscle relaxation, deep breathing) | High; can reduce anxiety and promote relaxation |
| Behavioral therapies (e.g., CBT-I) | High; addresses underlying sleep issues and negative thought patterns |
| Sleep hygiene practices (e.g., consistent sleep schedule, relaxing bedtime routine) | Moderate to High; improves sleep quality and reduces sleep disruptions |
Illustrations and Visual Aids
Understanding sleep paralysis requires a visual representation of the complex interplay between brain activity, sleep stages, and physiological changes. Visual aids can help clarify the often confusing and unsettling experience of sleep paralysis, making it easier to comprehend the underlying mechanisms.
Brainwave Patterns During Sleep Paralysis
Brainwave patterns during sleep paralysis are characterized by a transition between sleep and wakefulness. The brain’s electrical activity fluctuates rapidly, often showing a mixture of slow-wave sleep (delta waves) and faster, more desynchronized waves typical of wakefulness. This transition is crucial because it explains the feeling of being conscious while still being physically immobile. These patterns are not static but dynamic, fluctuating between different frequencies and intensities throughout the episode.
Typical Brain Activity Associated with Sleep Paralysis Episodes
Sleep paralysis is linked to specific areas of the brain, particularly those responsible for motor control and awareness. During an episode, the motor cortex, which initiates movement, may show activity inconsistent with the person’s inability to move. This is often accompanied by increased activity in the brain regions associated with alertness and fear response. The amygdala, a brain region processing emotions, plays a critical role in the anxiety often experienced during sleep paralysis.
Experiencing sleep paralysis can be really unsettling, marked by a feeling of being trapped and unable to move. It’s often accompanied by hallucinations and a sense of pressure on the chest. Fortunately, understanding these symptoms and implementing strategies like good sleep hygiene can help. For caregivers of loved ones with dementia, finding support and resources is key.
Seeking out helpful tips for dementia caregivers can provide valuable insights into navigating the challenges of caregiving, like managing behavioral changes and adapting routines. Ultimately, remembering these practical steps can ease the experience of sleep paralysis, allowing for better sleep and overall well-being.
The thalamus, which relays sensory information, might also be affected, leading to the vivid hallucinations that some people report.
Sleep Cycle and Stages of Sleep Paralysis
Sleep paralysis most frequently occurs during the transition between REM (Rapid Eye Movement) sleep and wakefulness. REM sleep is characterized by vivid dreams and increased brain activity. The transition from REM to wakefulness often disrupts the natural process, leaving the person conscious but unable to move. Sleep paralysis can happen during other stages, such as the transition from NREM (Non-Rapid Eye Movement) to wakefulness, but it’s less common.
Physiological Changes in the Body During Sleep Paralysis
Sleep paralysis is accompanied by physiological changes in the body. The body may experience a temporary paralysis of the voluntary muscles, preventing movement. Heart rate and breathing may increase as the body adjusts to the sudden transition between sleep and wakefulness. In addition, there’s often a surge in stress hormones, such as adrenaline and cortisol, contributing to the feeling of fear and anxiety associated with sleep paralysis.
Relationship Between Sleep Stages and Sleep Paralysis
| Sleep Stage | Characteristics | Sleep Paralysis Likelihood |
|---|---|---|
| REM Sleep | Rapid eye movements, vivid dreams, increased brain activity | High |
| NREM Stage 1 | Transition from wakefulness to sleep, light sleep | Low |
| NREM Stage 2 | Further sleep deepening, some brainwave activity | Low |
| NREM Stage 3 & 4 | Deep sleep, slow-wave activity | Very Low |
This table illustrates the stages of sleep and the relative likelihood of sleep paralysis occurring during each. The high likelihood during REM sleep transitions emphasizes the crucial role of this sleep phase in the experience.
Potential Complications and Long-Term Effects
Recurring sleep paralysis can significantly impact a person’s quality of life, extending beyond the immediate discomfort of the episodes themselves. The persistent nature of the experiences can lead to a cascade of psychological and potentially physical repercussions. Understanding these potential complications is crucial for effective management and support.
Long-Term Psychological Impact
Chronic sleep paralysis can create a substantial psychological burden. The fear and anxiety associated with these episodes can lead to significant distress and impair daily functioning. Individuals might experience heightened anxiety, panic attacks, and even post-traumatic stress disorder (PTSD) symptoms, especially if the episodes are frequent and intense. The unpredictability of sleep paralysis can contribute to a sense of vulnerability and powerlessness.
These feelings can manifest in a variety of ways, affecting an individual’s relationships, work performance, and overall well-being.
Influence on Mental Health
Sleep paralysis can act as a significant stressor, potentially exacerbating existing mental health conditions or contributing to the development of new ones. Anxiety disorders, depression, and PTSD are among the mental health concerns that can be exacerbated by sleep paralysis. The fear of future episodes and the disruption to sleep patterns can negatively impact mood regulation and emotional stability.
It’s important to note that the connection between sleep paralysis and mental health is complex, and not everyone who experiences sleep paralysis will develop a mental health condition.
Untreated Sleep Paralysis: Potential Complications
Leaving sleep paralysis untreated can lead to a range of problems. Prolonged periods of poor sleep quality, coupled with the fear and anxiety surrounding the episodes, can significantly impact overall physical and mental health. Untreated sleep paralysis may lead to difficulty concentrating, impaired memory, and a decline in cognitive function. The consistent disruption to sleep can also contribute to fatigue and reduced energy levels, affecting a person’s ability to perform daily tasks and maintain healthy relationships.
Potential Complications Table
| Potential Complication | Severity | Explanation |
|---|---|---|
| Anxiety and Panic Attacks | Moderate to Severe | Frequent sleep paralysis episodes can trigger or worsen anxiety and panic attacks, leading to significant distress and impairment in daily functioning. |
| Post-Traumatic Stress Disorder (PTSD) | Severe | In some cases, the overwhelming fear and terror associated with sleep paralysis can lead to the development of PTSD, requiring professional intervention. |
| Depression | Moderate to Severe | Chronic sleep deprivation and the psychological distress caused by sleep paralysis can contribute to feelings of hopelessness, sadness, and loss of interest, potentially leading to depression. |
| Sleep Deprivation | Moderate | Recurring episodes disrupt sleep patterns, leading to insufficient sleep and resulting in daytime fatigue, impaired concentration, and reduced alertness. |
| Cognitive Impairment | Moderate | Sleep deprivation and the associated anxiety can impact cognitive functions like memory, concentration, and decision-making. |
Final Review
In conclusion, sleep paralysis, while unsettling, is a relatively common experience. Understanding its symptoms, causes, and potential treatments is crucial for managing and reducing the fear and anxiety it can induce. The key takeaway is that sleep paralysis is often a temporary condition that can be effectively managed with a combination of lifestyle adjustments, relaxation techniques, and potentially, professional guidance.
This article has hopefully provided a clearer understanding of this often-misunderstood phenomenon.









