The timed up and go test (TUG) is a crucial assessment tool in various medical fields, especially geriatric care and neurological evaluations. It measures mobility and functional ability, providing valuable insights into a patient’s overall physical performance. This comprehensive guide dives into the details of the TUG test, from its definition and application to interpreting results and safety considerations.
Understanding the nuances of this test is essential for healthcare professionals and anyone interested in geriatric health or neurological conditions.
The TUG test involves a standardized procedure, with specific instructions and timing points. Different versions cater to varying populations and needs, from standard assessments to modified protocols. Factors like physical conditions, cognitive impairments, and medication can all impact a patient’s performance. Accurate interpretation of results is crucial for guiding treatment plans and monitoring progress over time.
Introduction to the Timed Up and Go Test (TUG)
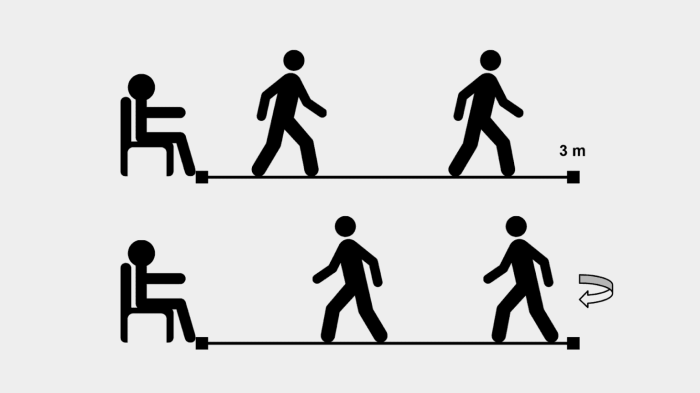
The Timed Up and Go (TUG) test is a simple yet effective assessment tool used to evaluate mobility and gait in individuals. It measures the time it takes a person to stand up from a chair, walk a short distance, turn around, and return to the chair. This practical test is valuable in various clinical settings, particularly for identifying potential fall risks and assessing functional abilities.The TUG test’s versatility lies in its application across diverse populations and clinical contexts.
It’s frequently employed in geriatric assessments to evaluate the risk of falls, which are a significant concern for older adults. Furthermore, the TUG test can be used to assess the impact of neurological disorders, such as stroke or Parkinson’s disease, on mobility. It provides clinicians with a quantitative measure of functional decline and can be used to track progress over time.
Equipment Needed for the TUG Test
The TUG test requires minimal equipment. A standard chair with a stable seat and back, typically of standard height for adults, is necessary. A stopwatch or timer for accurate timing is essential. A marked walkway of a specified length, such as 3 meters, is required for consistent measurements. The floor surface should be even and free of obstacles to ensure accurate and safe testing.
Finally, a designated space free of distractions is recommended to ensure a smooth test execution.
Different Versions of the TUG Test
The TUG test can be administered in various versions, each tailored to specific needs and patient populations. The standard TUG involves the individual rising from a chair, walking 3 meters, turning around, and returning to the chair. The modified TUG test, designed for individuals with more significant mobility limitations, often involves a support or assistance from a person to allow the test taker to accomplish the task.
| Version | Description | Specific Considerations |
|---|---|---|
| Standard TUG | Individual rises from a chair, walks 3 meters, turns around, and returns to the chair. | Assesses basic mobility in individuals with no or minimal mobility limitations. |
| Modified TUG | Individual rises from a chair, walks 3 meters, turns around, and returns to the chair with the assistance of a person or a support. | Assesses mobility in individuals with significant mobility limitations or impairments. |
Methodology and Procedure
The Timed Up and Go (TUG) test is a widely used assessment tool for evaluating mobility and fall risk in older adults. Understanding the precise methodology behind the test is crucial for accurate interpretation of results and reliable comparisons across different studies. A standardized procedure ensures that the test is administered consistently, minimizing variations and maximizing the validity of the outcome.The TUG test’s strength lies in its simplicity and practicality, allowing healthcare professionals to efficiently assess mobility in various settings.
Proper execution, however, is essential to produce meaningful data. This section delves into the detailed procedure, participant instructions, different measurement methods, and the importance of standardized protocols.
Step-by-Step Procedure
The TUG test involves a series of specific steps, each carefully designed to evaluate a participant’s ability to perform a common daily task – getting up from a chair, walking a short distance, and returning to the chair. The test begins with the participant seated in a chair. The examiner sets the timer and clearly communicates the instructions to the participant.
- The participant is instructed to rise from the chair, keeping their feet flat on the floor.
- The participant is asked to walk at a comfortable pace to a mark approximately 3 meters away.
- The participant is then instructed to turn around and walk back to the chair.
- The participant must sit down in the chair without assistance.
Participant Instructions
Clear and concise instructions are critical for consistent performance across participants. The examiner should provide specific guidance, avoiding ambiguity. The participant must understand what is expected during each phase of the test.
- The examiner should clearly articulate the need to maintain a normal walking pace, emphasizing neither rushing nor unduly slowing down.
- Participants must be encouraged to perform the task to the best of their ability.
- Important: The participant should not use any assistive devices, such as walking aids, during the test, unless specified in the study protocol.
Measuring Time
Different methods exist for recording the time taken during the TUG test. Accurate timing is crucial for reliable comparisons and data analysis. A stopwatch or a computerized timing system can be used.
- Stopwatches: Manual stopwatches offer a simple method but require careful attention from the examiner to start and stop the timer at the correct moments. The examiner needs to be focused on starting the timer as the participant stands up from the chair and stopping it when the participant sits down again. Manual errors can lead to inaccurate results.
- Computerized systems: Computerized systems offer a more precise and objective way to measure the time taken. These systems can automatically record the start and stop times, reducing the risk of human error and providing more reliable data.
Standardized Procedure Summary, The timed up and go test
Adhering to standardized procedures is paramount in the TUG test. This ensures comparability of results across different settings and studies.
| Step | Description | Timing Point |
|---|---|---|
| 1 | Participant seated in a chair | Start |
| 2 | Participant stands up | Timer starts |
| 3 | Walks 3 meters | – |
| 4 | Turns around | – |
| 5 | Walks back to chair | – |
| 6 | Participant sits down | Timer stops |
Importance of Standardized Procedures
Standardized procedures are crucial for ensuring the reliability and validity of the TUG test results. Consistent application of the test protocols minimizes variability in measurements, allowing for accurate comparisons and meaningful interpretation of the data. This is particularly important in clinical settings where the test is used to assess individual patient conditions and track progress over time.
The timed Up & Go test is a simple assessment of mobility, measuring how quickly someone can stand up, walk a short distance, turn around, and sit down again. However, for individuals with emetophobia fear of vomiting, this seemingly straightforward task can present a significant hurdle. The fear of losing control and potentially vomiting can significantly impact their performance on the test, even if their physical abilities are otherwise intact.
Ultimately, understanding the nuances of such tests and potential contributing factors like emetophobia is key for accurate interpretation and support.
Factors Affecting Performance
The Timed Up and Go (TUG) test, a common assessment of mobility, is influenced by a multitude of factors beyond just physical ability. Understanding these influences is crucial for accurate interpretation of results and appropriate intervention strategies. This section delves into the various factors that can impact TUG test performance, highlighting their potential effects on the measured time.The TUG test, while seemingly straightforward, is sensitive to a complex interplay of physical and cognitive conditions, as well as medication effects.
Each of these factors can significantly alter the time taken to complete the test, potentially misrepresenting a person’s true mobility capabilities. This understanding is critical in tailoring interventions to address specific needs.
Physical Conditions
Factors like balance issues, arthritis, and lower extremity weakness can substantially affect a person’s ability to navigate the TUG test’s physical demands. Difficulties with turning, stepping, and maintaining equilibrium can lead to increased time durations. For example, someone with severe osteoarthritis in their knees might experience significant pain and stiffness, impacting their speed and ability to perform the test accurately.
The level of severity of the physical condition and its impact on mobility are critical determinants of the test outcome.
Cognitive Impairments
Cognitive impairments, such as dementia or confusion, can also influence TUG test performance. Individuals with these conditions may struggle with the cognitive components of the test, such as understanding instructions, initiating movement, or maintaining focus during the task. The level of cognitive impairment can lead to longer times and potentially misclassify the person’s true mobility. For instance, a person with mild cognitive impairment might experience difficulty focusing on the instructions, leading to slower execution and longer completion times.
Medication Effects
Medications, including those for pain management, blood pressure control, and other conditions, can influence TUG test scores. Side effects such as dizziness, drowsiness, or impaired coordination can affect performance. For example, certain anti-hypertensive medications can lead to orthostatic hypotension, causing dizziness and unsteady gait, which would directly impact the TUG test time.
Potential Effects of Different Factors
| Factor | Potential Effect on TUG Time | Example |
|---|---|---|
| Balance Issues | Increased time due to difficulty maintaining equilibrium. | A person with vestibular dysfunction might take longer to complete the test due to unsteadiness. |
| Arthritis | Increased time due to pain and stiffness in joints. | Someone with severe knee arthritis might exhibit a significantly longer TUG time due to pain and limited range of motion. |
| Cognitive Impairment | Increased time due to difficulty with instructions or maintaining focus. | A patient with mild dementia might struggle to understand the instructions and take longer to complete the test. |
| Medications (e.g., sedatives) | Increased time due to dizziness, drowsiness, or impaired coordination. | A person taking a sedative might have difficulty with balance and coordination, leading to a longer TUG time. |
| Lower Extremity Weakness | Increased time due to difficulty with stepping and turning. | Someone with significant lower extremity weakness might have trouble taking steps or turning, resulting in an extended TUG time. |
Interpretation of Results
The Timed Up and Go (TUG) test provides valuable insights into a person’s mobility and risk of falls. Understanding how to interpret TUG results is crucial for clinicians and caregivers to develop effective interventions and monitor progress. Accurate interpretation involves considering the individual’s baseline, pre-existing conditions, and the context of the test environment.Interpreting TUG results requires a nuanced approach, recognizing that the same time taken can indicate different levels of functional impairment depending on the individual’s baseline and specific condition.
A score of 10 seconds might be considered normal for a healthy young adult, but it could signify significant impairment for an elderly person with Parkinson’s disease. Understanding the significance of different time ranges for various populations is key to proper assessment.
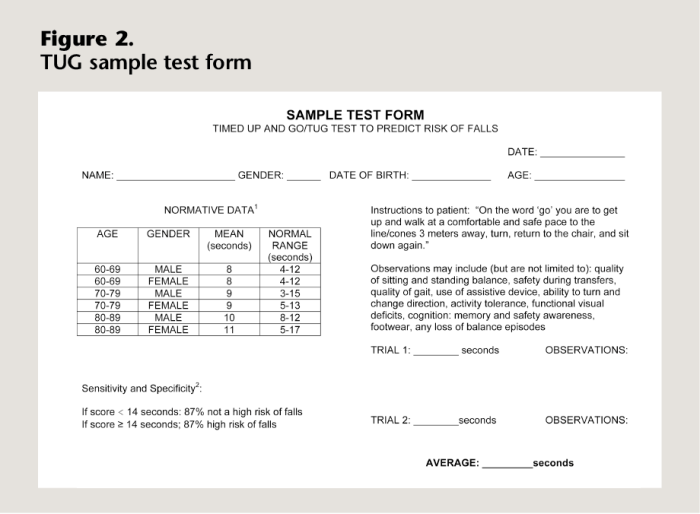
Significance of Time Ranges in Different Populations
Different populations have varying average TUG times. Age, gender, and pre-existing conditions all influence performance. A longer time suggests greater difficulty with mobility tasks, which could indicate a higher risk of falls or functional decline. For example, a healthy adult in their 30s with a TUG time of 10 seconds would be considered normal, whereas a similar time in a 70-year-old with arthritis might indicate a need for closer monitoring or intervention.
Understanding these differences is crucial for appropriate clinical judgment.
Clinical Interpretations Based on Time
This table Artikels typical TUG test scores and their corresponding clinical interpretations. Note that these are general guidelines, and individual circumstances should always be considered.
| TUG Time (seconds) | Clinical Interpretation |
|---|---|
| < 9 | Normal mobility; low fall risk |
| 9-12 | Slightly impaired mobility; moderate fall risk |
| 12-15 | Moderately impaired mobility; high fall risk |
| >15 | Significantly impaired mobility; very high fall risk |
Using TUG for Monitoring Functional Change
The TUG test is a valuable tool for monitoring functional change over time. By repeating the test at regular intervals, clinicians can track improvements or declines in mobility. For instance, a patient with a history of stroke who initially scored 20 seconds on the TUG might show improvement after physical therapy, achieving a score of 15 seconds after a few months.
This trend provides valuable data for adjusting treatment plans and ensuring the effectiveness of interventions. A consistent decrease in TUG time indicates positive progress, whereas a worsening trend signals the need for reevaluation and potential adjustments in care.
The timed Up & Go test is a simple yet effective way to assess mobility. It’s crucial for monitoring changes in physical function, and while I’m no expert on skin conditions, sometimes a sudden change in something like the appearance of a mole could indicate a need for a checkup. Learning more about what causes moles to suddenly appear might be helpful in understanding overall health, and in turn, this knowledge can be used to better assess how the timed Up & Go test results may change over time.
Understanding the reasons behind these changes is essential to properly interpreting the test results and potentially identify any underlying issues. what causes moles to suddenly appear Ultimately, both the timed Up & Go and any skin changes should be discussed with a doctor.
Examples of Treatment Plan Guidance
TUG results can directly inform treatment strategies. For example, if a patient with Parkinson’s disease demonstrates a TUG time of 18 seconds, the physical therapist might focus on exercises that improve gait, balance, and strength. Regular TUG testing allows the therapist to assess the effectiveness of the interventions and adjust the plan as needed. Similarly, for individuals with osteoarthritis, the treatment might involve pain management strategies, assistive devices, and exercises to maintain mobility and prevent further decline.
Applications and Variations
The Timed Up and Go (TUG) test has proven its versatility in assessing mobility and fall risk in various clinical settings. Its straightforward design and relatively quick administration make it a valuable tool for diverse patient populations. This section explores the diverse applications and variations of the TUG test, highlighting its adaptability and the reliability of its results across different contexts.The TUG test’s adaptability extends beyond its fundamental form, allowing for modifications tailored to specific patient needs.
These variations are crucial in ensuring accurate and meaningful assessments, particularly in individuals with impairments that might affect the standard test procedure. Reliability and validity of the TUG test are crucial considerations, especially when comparing results across different settings and populations.
Different Applications in Clinical Settings
The TUG test is widely used in a range of clinical settings to evaluate mobility and risk of falls. Its application extends from geriatric assessments to neurological evaluations and even rehabilitation programs. In geriatric care, it helps identify patients at risk of falls, enabling proactive interventions. In neurology, it can assess gait abnormalities and balance issues associated with various conditions.
In rehabilitation, the TUG can track progress and adjust interventions to optimize functional mobility.
Variations for Specific Populations
The TUG test has been adapted for various populations, such as children and individuals with visual impairments, to ensure accurate and meaningful assessments. These variations often involve adjustments to the testing environment or procedure. For example, a modified TUG for children might include a verbal cue to guide the child through the task, while a variation for individuals with visual impairments might incorporate verbal guidance and adjustments to the room’s lighting or visual cues.
The timed up and go test is a simple but effective way to assess mobility. Understanding how different pain medications, like Conzip vs Percocet, affect mobility is crucial for patients. Knowing the differences between these medications, as outlined in this helpful resource conzip vs percocet what s the difference , can be important when evaluating a patient’s overall functional ability, especially in relation to the timed up and go test results.
This test is often used in conjunction with other assessments to get a comprehensive picture of a person’s mobility.
Reliability and Validity of the TUG Test
The reliability and validity of the TUG test have been extensively studied across different populations and contexts. Studies show high test-retest reliability, indicating consistent results when repeated. Furthermore, the TUG’s validity, its ability to measure what it intends to measure, has been supported by correlations with other measures of mobility and fall risk. This suggests the test’s ability to identify individuals at risk of falls.
Comparison of TUG Test Versions
| TUG Test Version | Target Population | Key Modifications |
|---|---|---|
| Standard TUG | Adults (generally healthy or with mild mobility issues) | Standard procedure: rise from chair, walk 3 meters, turn around, return to chair. |
| Modified TUG for Children | Children (e.g., developmental disabilities, cerebral palsy) | Simplified instructions, visual cues, shorter walking distance, and verbal guidance. |
| TUG for Individuals with Visual Impairments | Individuals with visual impairments | Verbal guidance, clear auditory instructions, adjustments to lighting and visual cues. |
| TUG for Individuals with Neurological Conditions | Individuals with neurological conditions (e.g., stroke, Parkinson’s disease) | Careful observation of gait patterns, potential for modified walking distance, and potentially using assistive devices. |
Strengths and Weaknesses of the TUG Test
| Context | Strengths | Weaknesses |
|---|---|---|
| General Population | Simple to administer, relatively inexpensive, provides a quick assessment of mobility and fall risk. | May not capture subtle gait abnormalities or specific impairments, susceptible to environmental factors. |
| Children | Can be adapted for diverse needs, provides a measure of functional mobility. | Requires careful attention to developmental variations, and may require trained personnel to adapt the test. |
| Individuals with Visual Impairments | Can be adapted for specific needs, provides a measure of mobility in a challenging environment. | Needs careful consideration of the test environment and verbal guidance, may not be suitable for individuals with severe visual impairment. |
| Individuals with Neurological Conditions | Can provide insights into gait abnormalities, can track progress during rehabilitation. | Results might be affected by the severity and type of neurological condition, requires expertise in interpreting results. |
Data Presentation and Analysis: The Timed Up And Go Test
Presenting and analyzing Timed Up and Go (TUG) test data effectively is crucial for drawing meaningful conclusions and interpreting the results accurately. This involves choosing appropriate graphical representations and statistical methods to highlight trends, identify potential factors influencing performance, and compare different groups or conditions. The goal is to transform raw data into easily understandable visuals and quantifiable metrics that facilitate a deeper understanding of the test’s outcomes.Proper data handling and analysis contribute significantly to the validity and reliability of the study findings.
By meticulously organizing and representing the data, researchers can accurately assess the impact of various factors on the TUG test scores and draw valid conclusions from the observed trends.
Graphical Representations of TUG Data
Visual representations are essential for quickly understanding patterns and trends in TUG test data. Different graphs effectively convey different aspects of the data. Choosing the right graph is crucial for clear communication of the results.
- Box Plots: Box plots provide a concise summary of the distribution of TUG test times across different groups or conditions. They display the median, quartiles, and potential outliers. This visualization allows for a quick comparison of the central tendency and variability in performance. For example, comparing box plots of TUG times for individuals with and without Parkinson’s disease reveals potential differences in their performance characteristics.
- Histograms: Histograms show the frequency distribution of TUG test times. They group the data into bins and visually depict the concentration of scores within specific ranges. Histograms can reveal the shape of the distribution, whether it’s skewed or symmetrical. For instance, a histogram can illustrate how many participants took between 10 and 15 seconds, or between 15 and 20 seconds, to complete the TUG test.
This visualization helps to understand the spread of the data.
- Scatter Plots: Scatter plots are useful for examining relationships between TUG test times and other variables. Plotting TUG times against age, for example, can reveal if there’s a correlation between these factors. A scatter plot allows visualization of the relationship between variables, revealing if there is a positive or negative correlation. This type of visualization aids in the identification of potential patterns or trends in the data.
Statistical Analyses for TUG Data
Choosing the correct statistical analysis depends on the research question and the nature of the data. Common statistical tests for analyzing TUG test results include t-tests, ANOVA, and correlation analyses.
- T-tests: T-tests compare the means of two groups. For example, a t-test can be used to determine if there’s a significant difference in mean TUG times between a treatment group and a control group. This statistical method can be used to evaluate the effectiveness of a specific intervention on the TUG test performance.
- Analysis of Variance (ANOVA): ANOVA compares the means of three or more groups. It’s used to analyze differences in TUG times among various groups, such as individuals with different diagnoses or those receiving different treatments. ANOVA is particularly useful when assessing the effect of multiple factors on TUG performance.
- Correlation Analyses: Correlation analyses evaluate the strength and direction of the relationship between TUG test times and other variables, such as age, gender, or disease severity. This type of analysis helps to understand if a correlation exists between the independent and dependent variables.
Organizing Data for Analysis
Data organization is crucial for accurate analysis. Data should be structured in a clear and consistent manner, with each participant’s data organized in rows and variables in columns.
| Participant ID | Age | Gender | Diagnosis | TUG Time (seconds) |
|---|---|---|---|---|
| 1 | 70 | Female | Parkinson’s | 15.2 |
| 2 | 65 | Male | Parkinson’s | 12.8 |
| 3 | 82 | Female | Healthy | 8.5 |
This table format allows for easy data entry, manipulation, and analysis using statistical software.
Illustrative Case Studies
The Timed Up and Go (TUG) test, a simple yet powerful assessment tool, provides valuable insights into a patient’s mobility and risk of falls. Analyzing case studies allows us to see how the TUG test’s results can be used to inform personalized treatment plans and monitor progress. These examples highlight the clinical utility of the TUG test in various contexts.Understanding how the TUG test impacts diagnosis and treatment planning is critical for healthcare professionals.
Case studies offer a practical application of the test’s methodology, demonstrating its efficacy in real-world situations. They also illustrate how variations in patient characteristics and conditions can influence TUG scores, prompting careful consideration during interpretation.
Case Study 1: Assessing Mobility in Parkinson’s Disease
The TUG test is often employed in the assessment of individuals with Parkinson’s disease (PD), a neurodegenerative disorder impacting movement. A patient with a diagnosed history of PD presents with gait instability and freezing episodes.
| Assessment Date | TUG Time (seconds) | Other Relevant Data | Treatment Plan Adjustments |
|---|---|---|---|
| Baseline | 15.2 | Significant freezing episodes observed during the test. Symptoms of rigidity noted during movement. | Initiate physical therapy focusing on gait training, balance exercises, and strategies for managing freezing episodes. |
| 3 Months Follow-up | 12.8 | Freezing episodes less frequent, and gait more fluid. Improved rigidity observed. | Continue physical therapy, but incorporate strength training to improve overall motor function. Consider medication adjustments to manage PD symptoms. |
This case study demonstrates how the TUG test can be used to track improvements in mobility over time, allowing for adjustments to the treatment plan. The progressive decrease in TUG time indicates a positive response to the intervention, providing encouraging evidence for the efficacy of the treatment approach.
Case Study 2: Monitoring Post-Stroke Rehabilitation
Following a stroke, individuals often experience significant mobility impairments. The TUG test is invaluable in monitoring their recovery and adapting rehabilitation strategies.A patient experienced a moderate ischemic stroke affecting the right hemisphere. The patient presented with right-sided weakness and balance difficulties. Initial TUG time was 20.5 seconds.
| Assessment Date | TUG Time (seconds) | Other Relevant Data | Treatment Plan Adjustments |
|---|---|---|---|
| Baseline | 20.5 | Right-sided weakness; difficulty with balance and turning; notable slowness in movement. | Start with a focused rehabilitation program emphasizing exercises for upper and lower body strength, balance, and mobility. Speech therapy was also recommended. |
| 2 Months Follow-up | 17.1 | Right-sided weakness reduced, but still present. Balance improved. | Maintain the current rehabilitation plan and continue to focus on strength training and balance exercises. |
| 4 Months Follow-up | 14.8 | Right-sided weakness further improved. Balance now more stable. | Continue with rehabilitation, gradually increasing the intensity and complexity of exercises. Introduce activities to enhance functional mobility. |
The progressive decrease in TUG time, from 20.5 seconds to 14.8 seconds, clearly shows the impact of rehabilitation on the patient’s mobility. This detailed monitoring, facilitated by the TUG test, allowed for personalized adjustments in the treatment plan.
Safety Considerations
The Timed Up and Go (TUG) test, while a valuable assessment tool, requires careful consideration of safety protocols. Proper administration is paramount to ensuring the well-being of both the patient and the administrator. This section delves into crucial safety measures, specific precautions for patients with particular medical conditions, adaptations for diverse mobility levels, and potential risks in various settings.
Safety Measures for Administration
A comprehensive set of safety precautions is essential to mitigate potential risks during the TUG test. These precautions ensure the patient’s safety and comfort throughout the procedure.
- Clear and Safe Testing Environment: The testing area should be free from obstacles and hazards. This includes removing clutter, ensuring adequate lighting, and securing any loose items that could cause a fall. A clear path of at least 10 feet should be maintained for the patient to navigate during the test.
- Proper Supervision: A qualified healthcare professional should closely supervise the patient during the entire TUG test. The administrator should be positioned to react swiftly if the patient loses balance or experiences any distress.
- Patient Consent: Obtaining informed consent from the patient is crucial. The patient must understand the procedure and potential risks before commencing the test.
- Monitoring Vital Signs: If possible, monitoring vital signs (blood pressure, heart rate, etc.) before, during, and after the test is recommended, particularly for patients with underlying health conditions. This will allow for immediate action if any adverse reactions occur.
- Emergency Preparedness: Ensure a readily available emergency response system, such as a call button or access to medical assistance, is within reach throughout the testing area.
Precautions for Patients with Specific Medical Conditions
The TUG test may not be suitable for all patients, especially those with specific medical conditions. Careful consideration and adaptation are necessary.
- Cardiovascular Issues: Patients with unstable cardiovascular conditions should be evaluated for potential risks before performing the test. If there is concern, the test may need to be modified or avoided altogether. A medical professional should assess the appropriateness of the test.
- Neurological Conditions: Patients with conditions that affect balance or coordination (e.g., stroke, Parkinson’s disease) may require additional support or modifications to the test. The support should be tailored to the patient’s specific needs.
- Orthopedic Issues: Patients with recent orthopedic injuries or surgeries may require significant modifications to the TUG test. The test may need to be shortened, or alternative assessments may be more suitable.
Adapting the TUG Test for Mobility Limitations
Patients with significant mobility limitations may require modifications to the TUG test to ensure their safety and participation.
- Assistive Devices: Allowing the use of assistive devices such as walkers, canes, or wheelchairs is critical for patients with limited mobility. The use of such devices should be determined based on the patient’s needs and capabilities.
- Shortened Distance: The distance for the TUG test can be adjusted for patients with impaired mobility, reducing the distance if necessary. This adjustment is essential to prevent undue stress on the patient.
- Alternative Assessment: In cases where the standard TUG test is not feasible, alternative mobility assessments can be used. These alternatives may involve the patient’s walking capabilities or the ability to perform certain activities.
Safety Checklist for TUG Test
A comprehensive checklist is critical for ensuring both patient and administrator safety.
| Step | Action |
|---|---|
| 1 | Confirm patient consent and understanding of the procedure. |
| 2 | Ensure a safe testing environment with no obstacles. |
| 3 | Position administrator for close supervision and quick response. |
| 4 | Verify availability of emergency response system. |
| 5 | Document any assistive devices used. |
| 6 | Monitor patient vital signs (if applicable). |
| 7 | Observe patient for any signs of distress. |
| 8 | Terminate the test immediately if the patient experiences discomfort or loss of balance. |
Potential Risks in Different Contexts
The TUG test, like any assessment, carries potential risks. These risks can vary depending on the context of administration.
- Hospital/Clinic Settings: Risks are generally lower due to the presence of medical personnel and equipment.
- Home Health Settings: Potential risks may be higher, necessitating careful assessment of the home environment and the patient’s home support system.
- Community-Based Programs: Safety considerations need to address the specific environment and resources available.
Epilogue
In conclusion, the timed up and go test offers a practical and reliable method for evaluating mobility and functional ability. Its versatility across diverse populations and clinical settings makes it a valuable tool for healthcare professionals. This guide has explored the intricacies of the TUG test, from methodology and factors affecting performance to interpretation and safety measures. Understanding the TUG test is critical for delivering effective and personalized care, ultimately improving patient outcomes.










